Overview
Massachusetts General Hospital (MGH), part of Mass General Brigham, is a large teaching hospital located in Boston, Ma., that offers comprehensive telestroke and teleneurology programs to community hospitals.
Telestroke services provide smaller hospitals access to vascular neurologists 24 hours per day, seven days per week, to treat acute stroke and other emergency neurology conditions. Teleneurology services provide smaller hospitals access to neurohospitalists with a variety of different subspecialties, 24 hours a day, seven days a week, to treat urgent and routine neurology conditions.
Both services can be flexibly deployed in a wraparound model to cover the hours, days or weeks needed by the smaller hospital if local neurology coverage exists, and both include the option to enable local neurology services to leverage MGH’s technology and tools to provide virtual local coverage.
Strategic goals
MGH provides teleneurology and telestroke services through partnership with several community hospitals.
Strategic goals for MGH (hub hospital)
- Distribute MGH’s clinical expertise across its network through the standardization of clinical protocols and realtime decision support.
- Preserve inpatient capacity for patients with higher-acuity neurological conditions.
- Support expansion of the MGH network.
Strategic goals for community (spoke) hospitals
- Retain patients who would otherwise be transferred to MGH or another tertiary hospital.
- Improve availability of timely neurological consultation.
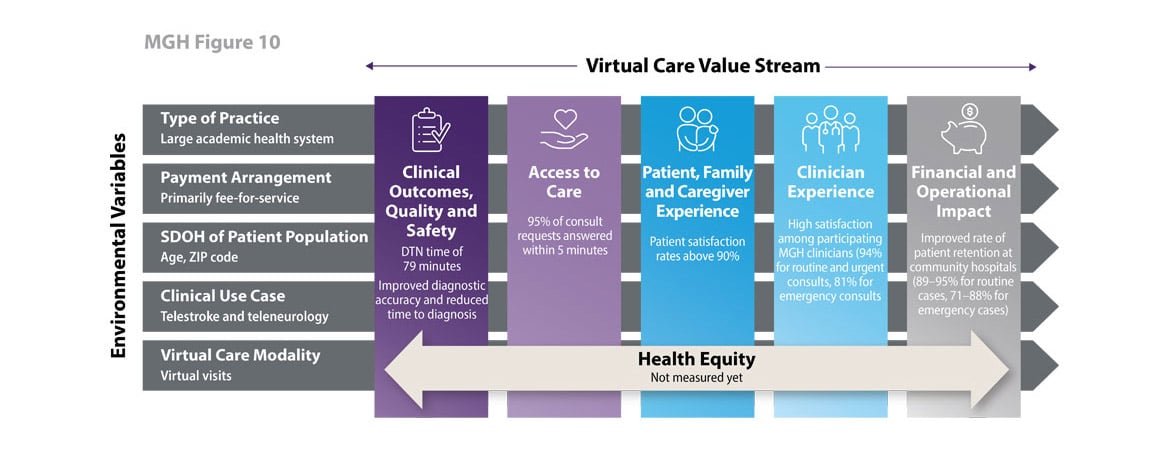
Program impact on health care value streams
In 2000, MGH pioneered using telestroke capabilities to help emergency physicians at a health system-affiliated institution, Martha’s Vineyard Hospital (MVH), to determine whether patients were experiencing an acute ischemic stroke and, if so, whether to administer a lifesaving drug—tissue plasminogen activator (tPA).
Initial successes generated by the program at MVH and changes in the state’s regulatory environment1 that supported expansion of the telestroke model enabled MGH to grow and develop a robust huband-spoke specialty telestroke and teleneurology network, which now includes 34 community hospitals.
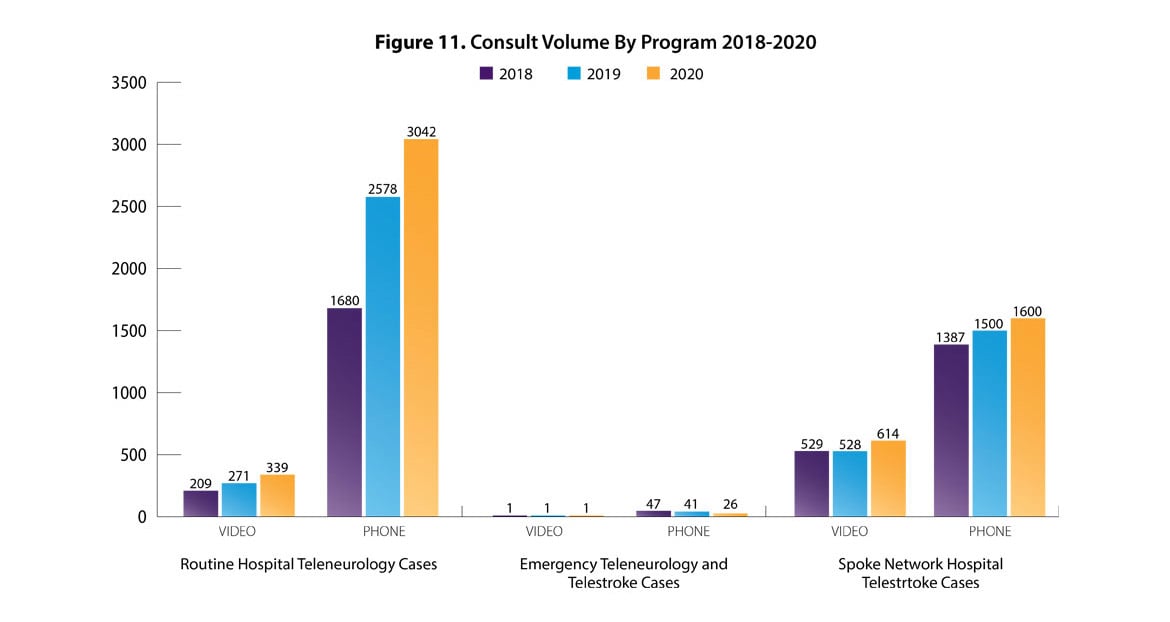
Demographic data specific to the telestroke program indicate that the program serves a predominantly older population; nearly 90% are over age 50, and the median age is 70 years old. Telestroke patients are relatively evenly split by gender. There are about 15 physicians providing telestroke consults and 12 physicians providing teleneurology consults across all the participating hospitals. These consulting physicians provide several thousand consults per year to community hospitals, many of which no longer have on-site neurologists.
MGH offers participating community hospitals support through:
- 24/7 access to phone or videoconferencing technology to enable remote examination of the patient.
- Review of brain scan images and other clinical data to inform decision-making related to stroke or neurological care.
- Implementation support for new sites with mock code stroke drills.
- Access to prerecorded continuing medical education (CME) and nursing-accredited Grand Rounds lecture series.
- Ongoing technical support and clinical support by an experienced nursing leader who serves as a clinical liaison to the program.
- Support from augmented intelligence (AI) applications for the assessment of large strokes or other complex vascular neurology conditions2.
1 In 2005, the Massachusetts Department of Public Health issued regulations requiring that ambulance personnel bring a patient who exhibited stroke-like symptoms to a certified “Primary Stroke Center” to be evaluated as a candidate for tPA. One requirement for certification was that a licensed physician with acute stroke expertise must be available on a 24/7 basis. Hospitals that lacked 24/7 neurology coverage could use a service such as telestroke to satisfy this rule.
2 For more information on the AMA’s AI policy.
Clinical outcomes, quality and safety
Door-to-needle time: Research analyzing data submitted by 16 of the MGH telestroke network’s spoke hospitals on tPA-treated patients from 2006 to 2015 found that hospitals treated a median of 13.5 patients with tPA per year; median hospital-level door-to-needle (DTN) time was 79 minutes, close to the recommended time of within 60 minutes. The greater the number of telestroke consults to the MGH, the greater the number of tPA treatments observed. In addition to improvements in DTN time, MGH has demonstrated improved diagnostic accuracy and reduced time to correct diagnosis as part of its telestroke program.
Access to care
Time to consult: Recent results over the past two years show that over 95% of consultation requests are answered within five minutes.
Patient, family and caregiver experience
- Patient satisfaction (at community hospitals): The program reports patient satisfaction rates above 90%.
Clinician experience
- Clinician satisfaction (at MGH): On average, participating clinicians report high satisfaction rates (scoring above 4 on the Hub Satisfaction Survey) of 94% over the past two years for routine and urgent consults and 81% for emergency consults.
- Clinician confidence/satisfaction (at community hospitals): Consultation support by MGH neurologists bolsters spoke hospital clinicians’ decision-making confidence, as the consulting MGH neurologist assumes responsibility for the recommendations.
Financial and operational impact
- Patient retention (at community hospitals):
- Routine or urgent cases: Between 2018 and 2020, the percentage of routine teleneurology patients who remained in the spoke hospital as a result of consultation ranged from 89% to 95%.
- Emergency cases: For emergency teleneurology and telestroke patients, between 71% and 88% were able to be treated locally with consultation support over the same period.
- Reduced patient/family cost: Costs are lower in community hospital settings, generating cost savings for patients and families.
Source: Data and content for this case study were provided by and used with permission from Massachusetts General Hospital.
Download the case study (PDF) and read other Return on Health telehealth case studies and scenarios.