Overview
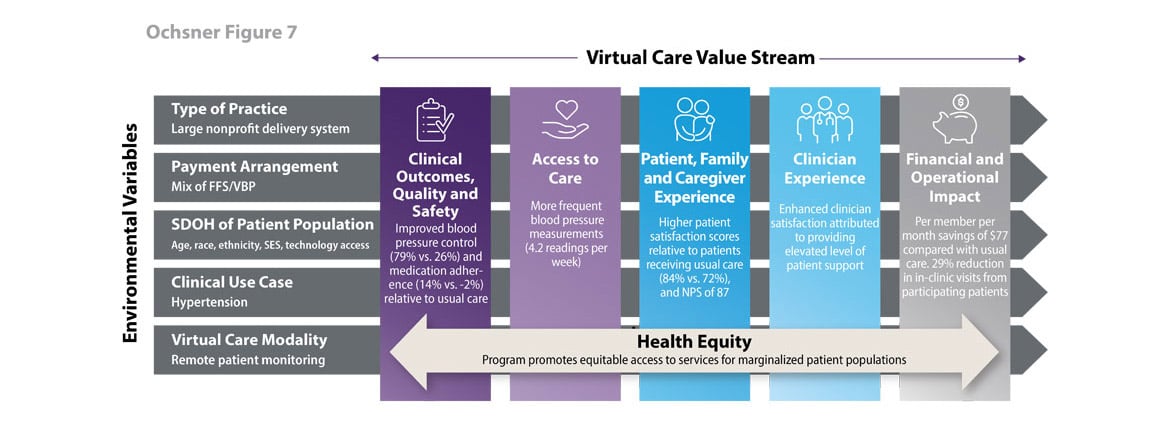
Ochsner Health System is a nonprofit, academic, multi-specialty, integrated delivery system based in New Orleans, LA, that serves over 700,000 patients a year.
Ochsner employs over 1,200 physicians and operates over 90 clinics and 20 hospitals.
Strategic goals
Ochsner utilizes its Hypertension Digital Medicine Program to:
- Improve clinical outcomes for patients with uncontrolled hypertension.
- Reduce avoidable emergency department and inpatient utilization by improving hypertension control.
- Improve primary care capacity.
Program impact on health care value streams
In 2015, Ochsner launched the Hypertension Digital Medicine Program, which provides digitally enabled chronic disease management to patients with hypertension, in an effort to address Louisiana’s high rates of hypertension.
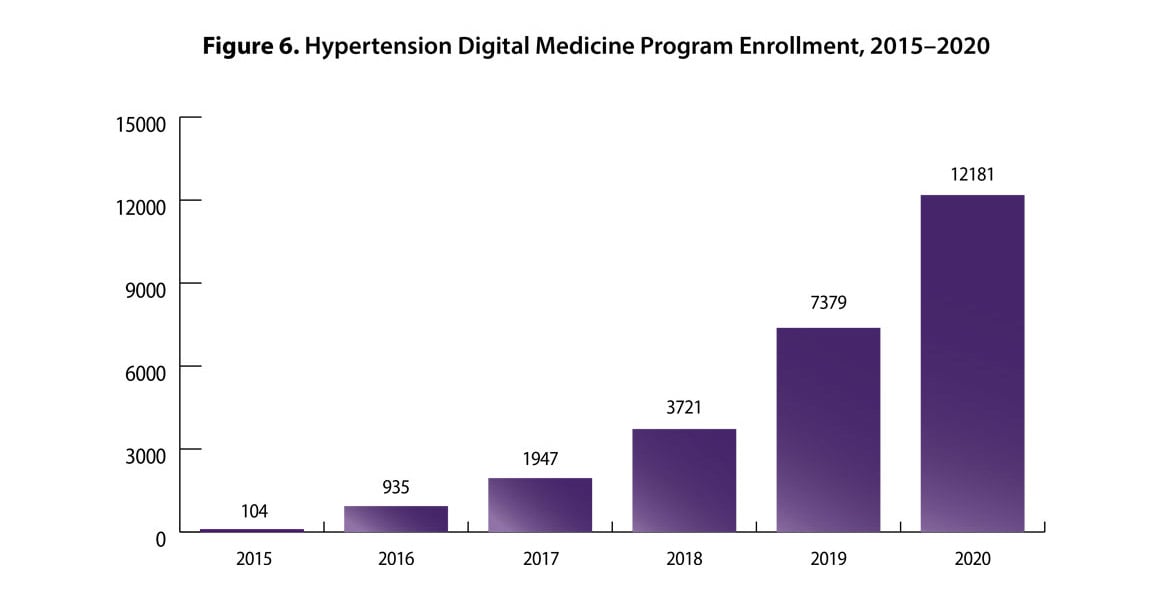
The program provides highly tailored, adaptive care to help program enrollees improve hypertension control rates. The program now serves approximately 13,000 individuals across 10 states. More than half of program enrollees are over 65 years old (65%), are women (55%) and identify their race or ethnicity as white (65%). Approximately, 33% of the program enrollees identify as Black and 2% identify as other. Program enrollment has increased more than 11,000% since the program launch (see Figure 6).
Ochsner has plans to expand the program to all 50 states in 2021.
Each program enrollee is assigned a dedicated care team (clinician, pharmacist and health coach) responsible for providing education, medication reconciliation and management and lifestyle recommendations according to established hypertension treatment guidelines. In addition, custom visual tools developed within the electronic health record (EHR) display the enrollee’s social needs, trending blood pressure over time, hypertension-related comorbidities, patient activation level, health literacy and relevant lab results that assist in optimizing the effectiveness and efficiency of the care team.
Program enrollees are asked to submit at least one blood pressure reading per week. If the care team has not received a reading from an enrollee for eight days, the enrollee receives an automated text reminder that a blood pressure measurement is needed. Care team members contact enrollees regularly by phone and review blood pressure measurement readings and treatment options for improving blood pressure control.
Enrollees are encouraged to work with the care team to co-create the treatment plan by choosing among various lifestyle and medication options. Each enrollee receives a monthly report (PDF) informing them of their progress in the program and tips for achieving better blood pressure control. Information about the enrollee’s progress is also available to their primary care provider.
Clinical outcomes, quality and safety
- Blood pressure control: Program enrollees achieved greater blood pressure control compared with a propensity-matched group that received usual care (79% versus 26%).
- Medication adherence: Medication adherence improved 14% among patients in the Digital Medicine Program and declined 2% among patients receiving usual care over the evaluation period of six months.
Access to care
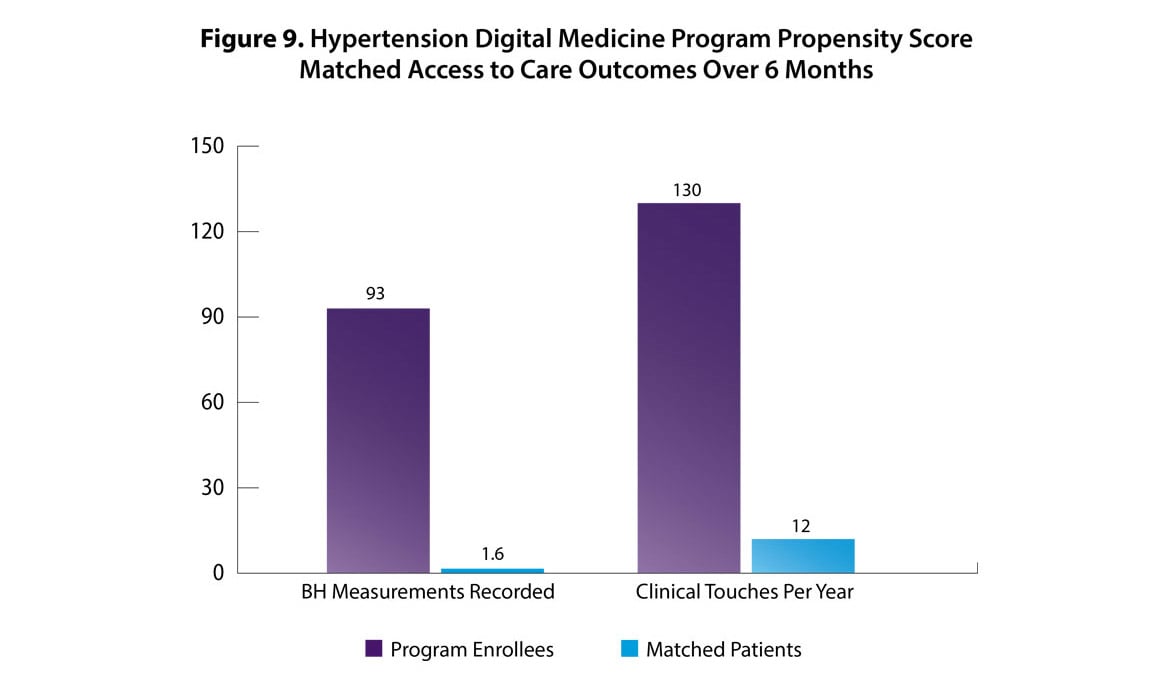
Clinical touches: Program enrollees had more frequent interactions with their care team (see Figure 9), and more blood pressure measurements recorded in the EHR compared with matched patients assigned to usual care. Current enrollees submit, on average, 4.2 blood pressure readings per week.
Patient, family and caregiver experience
- Patient satisfaction ratings: Program enrollees exhibited higher levels of satisfaction compared with matched patients who received usual care (84% versus 72%).
- Net Promoter Score: (NPS) increased from 77 in January 2020, prior to the launch of the mobile integrated care program, to 91 in January 2021.
Clinician experience
Clinician satisfaction: The program has enabled Ochsner’s primary care clinicians to provide an elevated level of support to patients, which has enhanced clinician satisfaction. When reflecting on how useful the program had been in a primary care setting, Ochsner’s chair of primary care noted to the leader of the Digital Medicine Program, “We forgot what help looked like.”
Financial and operational impact
- Per member per month cost impact: The program saves $77 per member per month compared with usual care. Based on these savings, Ochsner has contracts with several payers and employers who fully cover the costs of the program for their members or employees and, in some cases, even waive copays for program enrollees’ hypertension medications.
- Primary care provider capacity: A recent evaluation found that primary care physicians experienced a 29% reduction in the number of in-clinic visits from participating patients. Primary care clinicians reported the program helped reduce their workloads and enabled them to expand access to other patients.
Health equity
Equitable access to care: Ochsner has specifically designed the program to promote equitable access to its services for older patients, those with lower incomes, those facing social determinants of health inequities, and those with less prior experience using technologies provided in this program:
- The program is free to all patients, and some patients have their hypertension medication costs waived.
- Devices are mailed to patients or provided at the O Bar, a network of Ochsner retail locations which provides hands-on technical support and setup assistance for patients who lack access to or are unfamiliar with using technology.
- The program’s focus on incorporating assessment of social needs in the initial screening and ongoing progress reporting helps improve care team understanding of structural barriers to patient health.
Source: Data and content for this case study were provided by and used with permission from Ochsner Health.
Download the case study (PDF) and read other Return on Health telehealth case studies and scenarios.