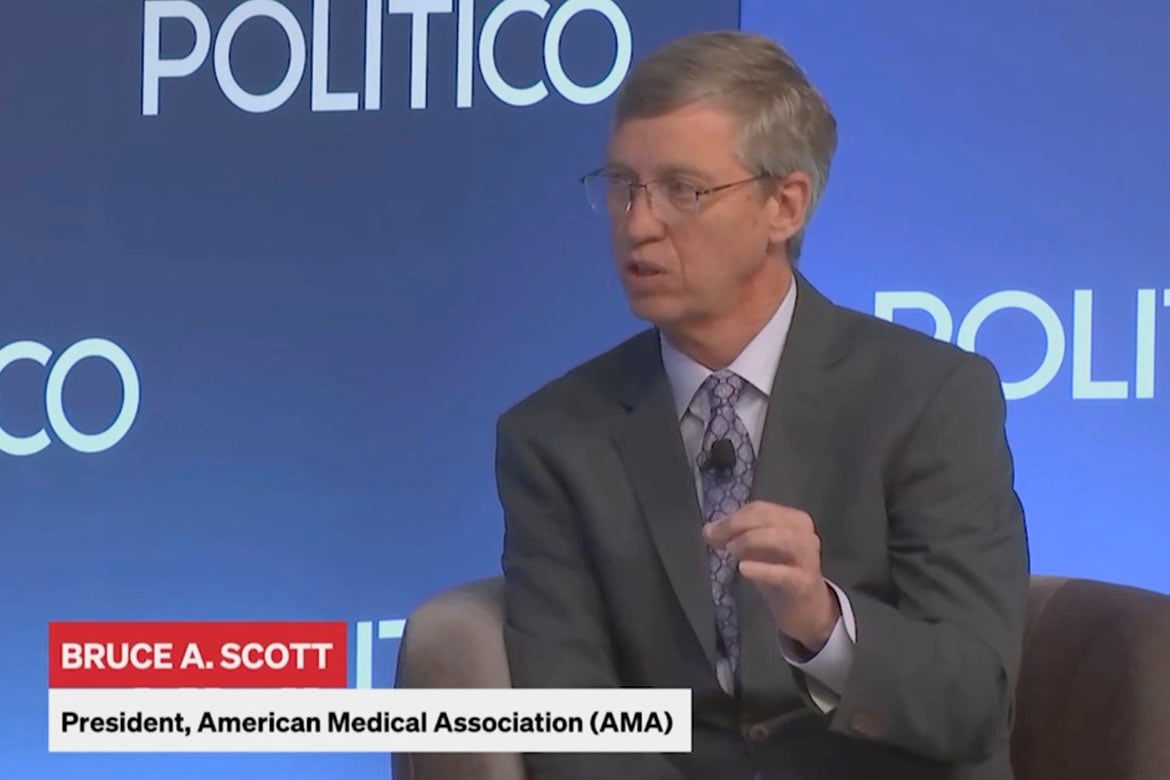
In a wide-ranging talk with reporter Kelly Hooper of Politico, AMA President Bruce A. Scott, MD, said he is holding out hope that the 2.8% Medicare pay cut physicians were dealt on Jan. 1 can be rolled back before the end of the year. That cut comes in a year where the Centers for Medicare & Medicaid Services (CMS) expects it to cost 3.5% more for physicians to provide care to the nation’s 66 million Medicare patients.
Dr. Scott also is hoping that Congress will pass legislation that would provide the long-term Medicare payment fix that physicians need so they can be confident that they are going to be able to financially sustain their practices.
Increasingly, physicians are being forced to turn away new Medicare patients, stop taking Medicare patients altogether or, in the worst-case scenarios, close or sell their practices. That is because—when adjusted for inflation—a 33% drop in Medicare pay (PDF) over the past 24 years has made staying in practice financially unsustainable.
“Physicians are struggling, and I really fear for access to care for our senior citizens,” Dr. Scott said.
There’s a reason to be nervous about the prospect of those two things happening this year given that physicians at the end of 2024 saw “left on the cutting room floor” a piece of legislation that had bipartisan support that would have rolled back the 2.8% cut and begin to link physician pay to the cost of care. And physicians were again disheartened this spring after being told during the continuing resolution budget discussions that they were going to get the fix their practices so desperately need only to see it get cut again.
“A lot of the reason for it—getting cut—was not because there is not bipartisan support, because I think there really is, but because of the desire to keep the packages skinny, if you will,” Dr. Scott told Hooper at the Politico Health Care Summit 2025. “Now it’s time for us to push forward with what is right: That physicians in America who are struggling to take care of their Medicare patients basically need a cost-of-living increase which they haven’t gotten in 24 years.”
The April summit brought together lawmakers, federal agency heads and industry leaders to discuss the health care landscape, policies and more.
Dr. Scott said he hopes that Congress will pass legislation that already has earned more than 150 co-sponsors from lawmakers on both sides of the aisle. Reps. Greg Murphy, MD (R-N.C.), and Jimmy Panetta (D-Calif.) and a bipartisan group of legislators earlier this year reintroduced the “Medicare Patient Access and Practice Stabilization Act,” H.R. 879.
If passed, the bill would cancel the 2.8% payment cut that took effect Jan. 1. It also would provide a 2% payment update. The AMA is urging physicians to contact lawmakers to tell them it is urgent to pass the bill.
A matter of time
Dr. Scott said he recognizes that there is a line-item cost of passing legislation, but he asked lawmakers to consider: “What is the cost of not fixing this?”
“We have a projected shortage of 86,000 physicians in 10 years. In many areas there is already a shortage of physicians. There are hundreds of counties in the United States that have no obstetrician, no primary care doctor, where the nearest physician in a specialty is 100-plus miles away,” he said. “It takes eight to 10 years to train a new physician, so if we don’t address this problem today, we’re not going to be in a good position 10 years from now when we are facing that shortage.”
Dr. Scott noted that Medicare’s trustees and the Medicare Payment Advisory Commission (MedPAC) support taking action to update physician payment, as does every lawmaker in Congress with a medical background.
“It is time for the rest of the legislators to listen to people who are knowledgeable about the system and recognize that change needs to occur,” he said.
Long-term fix needed
H.R. 879 helps physicians this year, but the physician payment formula also needs a more permanent fix, one that links the payment formula to the cost of providing care.
Hospitals, ambulatory surgery centers, long-term care facilities and essentially everyone else in Medicare already gets an inflation-based update. But not physicians.
“Physicians are the foundation of health care and yet we don’t get the update,” Dr. Scott noted. “If there are no physicians to provide care, how is there Medicare? It just doesn’t make any sense.”
Dr. Scott added that physicians need to know their practices will be sustainable.
“This isn’t some radical idea,” he said. “It basically puts physicians on par with all the rest of the providers … It makes sense to put the physicians on that same platform of giving us something for the future that we know we can look to and say it will be sustainable and I will be able to keep my practice alive.”
Explore further with the AMA’s Medicare Basics series, which provides an in-depth look at important aspects of the Medicare physician payment system.
Also, visit AMA Advocacy in Action to find out what’s at stake in reforming Medicare payment and other advocacy priorities the AMA is actively working on.