- Take action now: Contact Congress
- Medicare basics
- Current system is unsustainable
- Download Medicare payment graphics
- Medicare Conversion Factor, 2020-2025
- Medicare provider updates for 2025
- Medicare updates compared to inflation
- Key measures of practice expense, Medicare Economic Index
- Medicare spending per enrollee
- Real (inflation-adjusted) Medicare physician spending per enrollee
- Principles for Medicare physician payment reform
- The AMA fights Medicare cuts
The AMA is deeply alarmed about the growing financial instability of the Medicare physician payment system due to a confluence of fiscal uncertainties physician practices face related to the pandemic, statutory payment cuts, lack of inflationary updates and significant administrative burdens.
Take action now: Contact your members of Congress
Tell Congress to support legislation that would prospectively cancel the 2.83% payment cut that went into effect on January 1, while also providing a 2.0% payment update, helping to stabilize physician practices and protect patients' access to care. Use these materials in conversations with members of Congress to let them know the Medicare physician payment system needs reform to become a more sustainable, value-based system that better meets the needs of patients and physicians.
- The need for Medicare payment reform (PDF)
- Medicare alternative payment models (PDF)
- The principles: Characteristics of a rational Medicare physician payment system (PDF)
- Merit-based Incentive Payment System (MIPS): Problems and solutions (PDF)
Learn about how you can take part in the fight to fix Medicare on behalf of your patients and practices at the AMA's Fix Medicare Now website.
Medicare basics
- Medicare physician payment adequacy: Budget neutrality
- Merit-based Incentive Payment System (MIPS)
- The Medicare Economic Index
- Advancing value-based care with alternative payment models
- Transitioning to value-based care: Clinical data registries
- MIPS data problems
The AMA's Medicare Basics series provides an in-depth look at important elements of the Medicare physician payment system. Find more topics about the payment system and why it's in need of reform.
Current system is unsustainable
The evidence is clear: The Medicare payment system is on an unsustainable path threatening patient access to physicians.
Download Medicare payment graphics
Download and print the charts to use for your advocacy efforts.
Medicare Conversion Factor, 2020-2025
Medicare provider updates for 2025
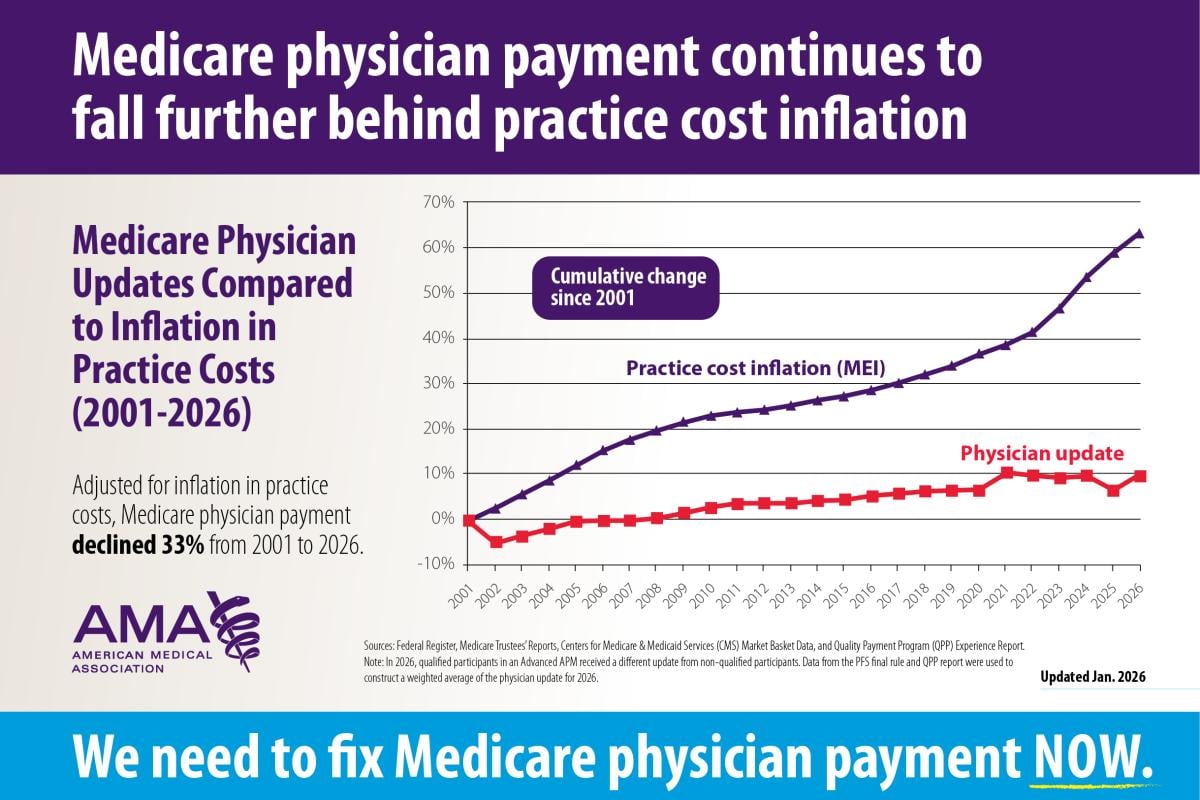
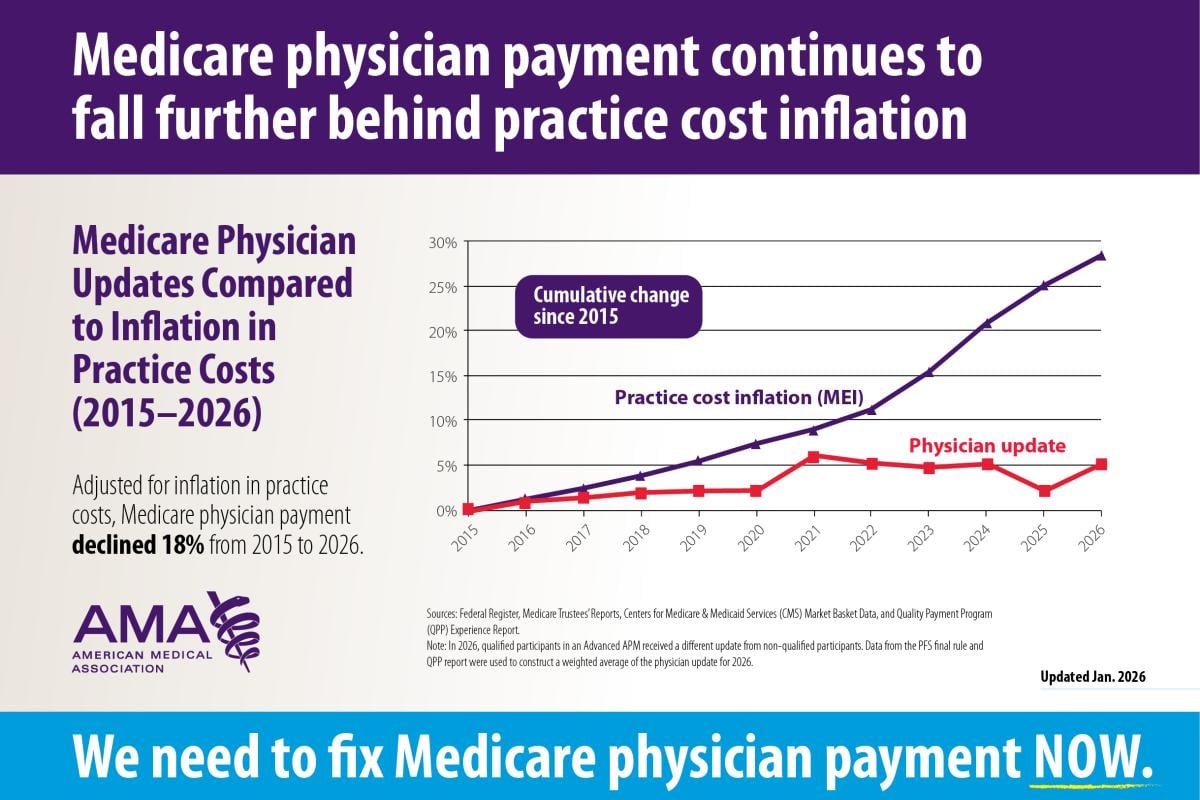
Medicare updates compared to inflation
2001-2026
2015-2026
Key measures of practice expense in the Medicare Economic Index
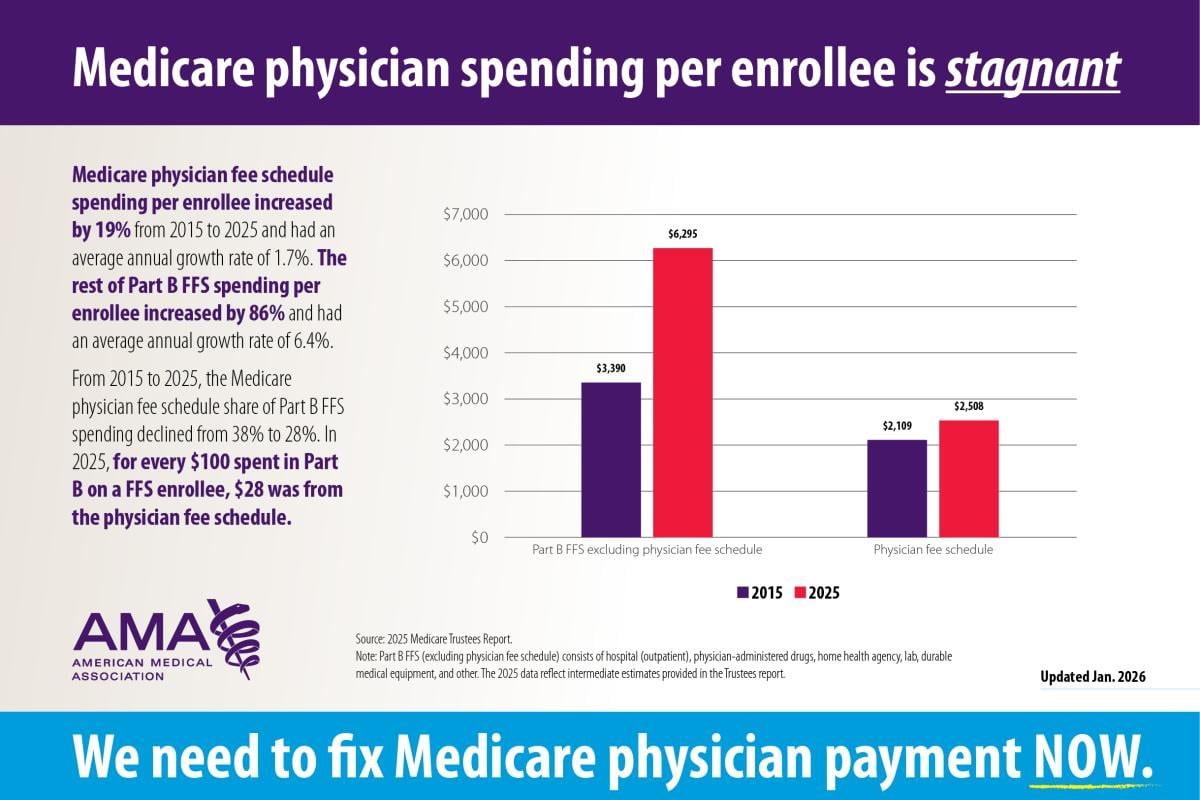
Medicare spending per enrollee
Real (inflation-adjusted) Medicare physician spending per enrollee
Principles for Medicare physician payment reform
The AMA and the Federation of Medicine have developed a set of principles to guide advocacy efforts on Medicare physician payment reform. Learn more.
The AMA fights Medicare cuts
Learn more about how the AMA fights against Medicare cuts, defending practices & access to care.