Creating medical education for the future
The AMA launched the "Accelerating Change in Medical Education" initiative in 2013. After initially awarding grants to 11 medical schools from across the country, the AMA brought these schools together to form the AMA Accelerating Change in Medical Education Consortium—a unique, innovative collaboration that allowed for the sharing and dissemination of groundbreaking ideas and projects.
The AMA added another 21 schools in 2016 and five more schools in 2019. Also in 2019, the AMA launched a new six-year, $15 million Reimagining Residency grant program with a goal of transforming residency training to best address the workplace needs of our current and future health care system. Eleven grant teams were selected to join the Accelerating Change in Medical Education and innovate graduate medical education across competency-based medical education, health systems science, transitions, the learning environment and workforce development. Collectively, members of the Accelerating Change in Medical Education Consortium made vast contributions to the future of medicine and worked to transform medical education across the continuum to create a system that trains physicians to meet the needs of today's patients and anticipate future changes.
View a timeline of work and milestones from the Accelerating Change in Medical Education initiative and download the list (PDF) of Accelerating Change in Medical Education Consortium schools and Reimagining Residency project teams (2013-2022).
The consortium has moved onto its next phase and become the ChangeMedEd Consortium. The Reimagining Residency projects are ongoing, and a new cohort of medical schools will be announced soon to continue the AMA’s transformative work in medical education.
View a video celebrating the decade of the Accelerating Change in Medical Education Consortium’s work
The following topics are an overview of some of the areas that projects associated with the Accelerating Change in Medical Education Consortium addressed from 2013-2022, although many projects cross more than one area.
Teaching new content in health systems science
Institutions in the consortium—Warren Alpert Medical School of Brown University, Mayo Clinic Alix School of Medicine, Brody School of Medicine at East Carolina University, Eastern Virginia Medical School, A.T. Still University-School of Osteopathic Medicine in Arizona, University of California, Davis, School of Medicine, University of Pittsburgh School of Medicine and other consortium members—implemented instruction in health systems science (HSS), the third pillar of medical education, along with the basic and clinical sciences.
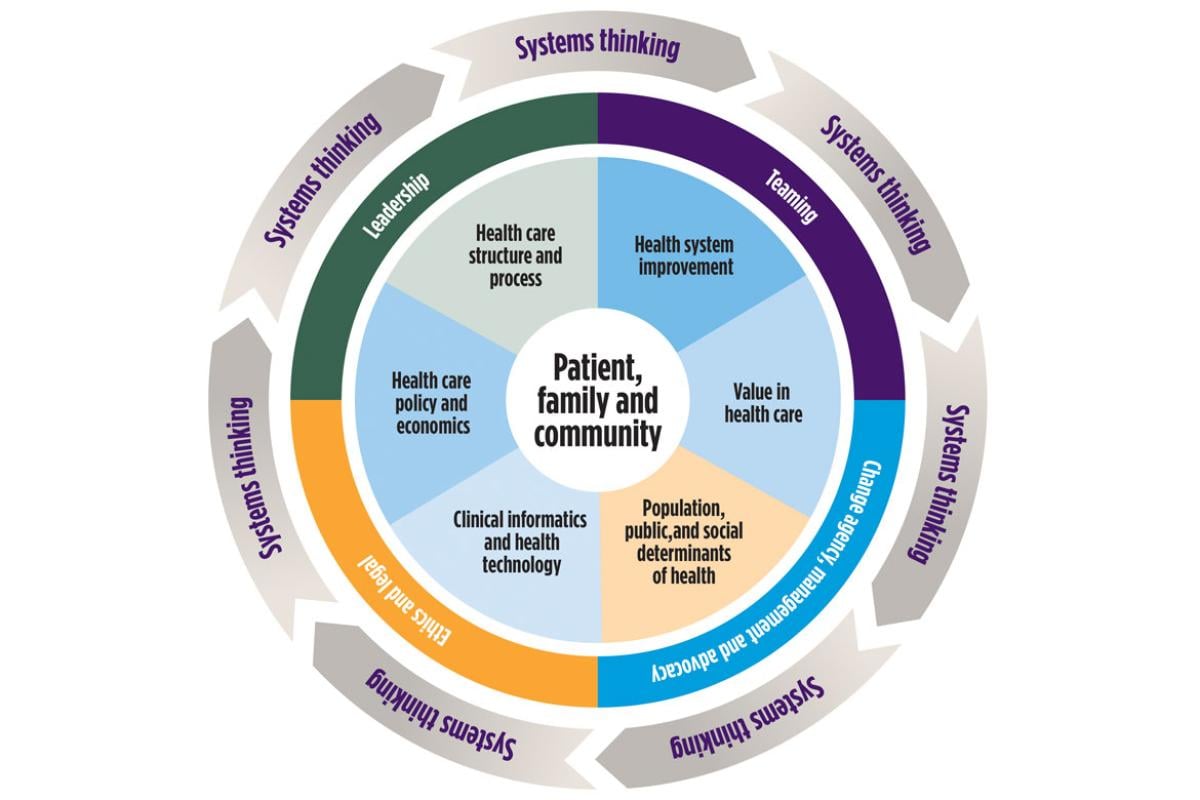
HSS is defined as a foundational platform and framework for the study and understanding of how care is delivered, how health professionals work together to deliver that care and how the health system can improve patient care and health care delivery.
The projects of several consortium member schools—University of Chicago Pritzker School of Medicine, Michigan State University College of Osteopathic Medicine and Emory University School of Medicine—specifically focused on the HSS domains of patient safety and quality improvement.
Projects at the University of Nebraska Medical Center College of Medicine, CUNY School of Medicine and Florida International University Herbert Wertheim College of Medicine focused more on teaching medical students to work as members of an interprofessional team, another HSS domain.
Envisioning the master adaptive learner
Preparing today's medical students for careers in the changing health care system requires more than clinical skills. They must be master adaptive learners. This means they have developed the adaptive expertise they need to deliver high-quality health care. They are expert, self-directed, self-regulated and lifelong workplace learners.
- Several consortium members, including Vanderbilt University School of Medicine, the University of Michigan Medical School and New York University School of Medicine, developed the Master Adaptive Learner model.
- Vanderbilt and Harvard Medical School are two of the consortium schools with consortium projects focused on implementing the Master Adaptive Learner model.
Developing flexible, competency-based pathways
Several consortium members, including Oregon Health & Science University, Ohio University Heritage College of Osteopathic Medicine and Virginia Commonwealth University School of Medicine implemented competency-based medical education. This means some students may move through medical school more quickly.
For example, a medical student who has already been educated and worked as a nurse, physician assistant or other health professional may need less time with the portions of medical school that are duplicative of their earlier training. Others may need more time to address deficiencies, better absorb learning or develop skills to become good physicians.
Working with health care delivery systems in novel ways
Penn State College of Medicine, Case Western Reserve University School of Medicine, Rutgers Robert Wood Johnson Medical School and the University of North Carolina School of Medicine are some of the consortium members that implemented value-added roles for medical students. These roles frequently involve partnerships with the health system and add value to the health system and to a student’s education.
Value-added roles for medical students are critical because health care payment is moving away from volume-based reimbursement to a system that prioritizes value. This means assessing and managing cost and value in health professions education is critical.
The University of Utah School of Medicine, another consortium member school, adapted tools developed by the University of Utah Health Sciences Center proven effective at bending the cost curve of health care to create a new educational model that emphasizes cost reduction and improves educational outcomes.
Making technology work for learning
Consortium member schools made technology work for learning. For example,
- Indiana University School of Medicine created a teaching electronic medical record system that has been implemented at the University of Connecticut School of Medicine and Sidney Kimmel Medical College at Thomas Jefferson University.
- Other consortium institutions such as the University of Texas Rio Grande Valley School of Medicine and the University of North Dakota School of Medicine and Health Sciences identified ways to use technology to address population health, cross communication barriers and increase access to care.
- The University of Washington School of Medicine used technology to integrate curricular change across the member institutions of WWAMI, a regional medical educational cooperative that operates in five states across three time zones.
- Stanford University School of Medicine developed a virtual reality curriculum that provides an immersive and safe environment to educate fellows and residents on diversity and inclusion.
- The University of Southern California Keck School of Medicine created an online digital health literacy curriculum for the medical education continuum.
Shaping tomorrow's leaders
Physicians need the skills to lead change that will shape the modern health care system, improve outcomes and reduce disparities.
Consortium schools—such as the University of California, San Francisco, School of Medicine, Dell Medical School at the University of Texas at Austin and others—integrated leadership training into curricula that prepares today's medical students to become future leaders.
Additionally, another consortium member, Morehouse School of Medicine, built and strengthened its diversity pipeline and mentoring support. Approximately 75 percent of its students are from groups underrepresented in medicine. This consortium member increased its class size and created a curriculum that allows for strong faculty-student interactions with longitudinal supervision by a limited number of faculty.
Another consortium school, the University of California, Irvine, School of Medicine, developed #MDsToo, a student mistreatment prevention curriculum for faculty and residents.