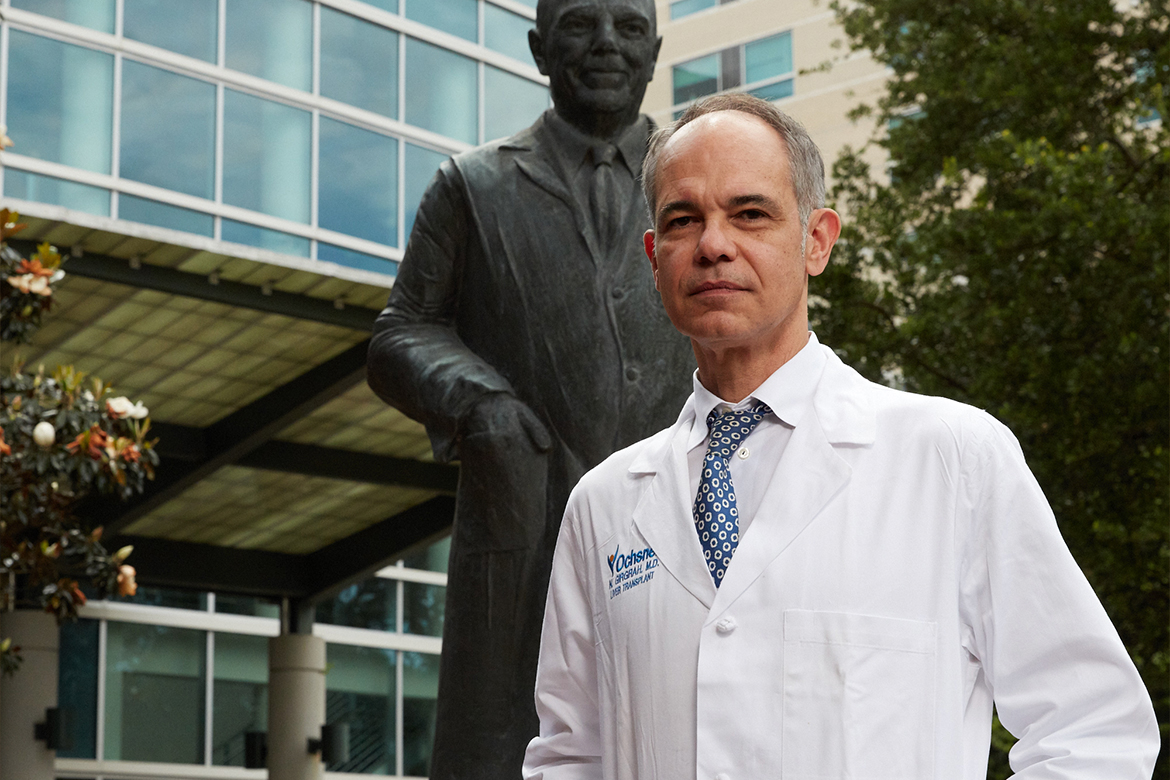
It started in May 2017 with a letter from the chief executive officer of Ochsner Health System in New Orleans expressing a call to action to address physician burnout. Three months later, the health system launched a provider well-being task force led by Nigel Girgrah, MD, a transplant hepatologist and medical director of the Ochsner Multi-Organ Transplant Institute.
One year after leading the taskforce, Dr. Girgrah reported findings to the executive team, expressing strongly that Ochsner needed a chief wellness officer and office of professional well-being to specifically focus on issues surrounding burnout.
The executive leadership team agreed and asked Dr. Girgrah to fill the vital new role.
“Dr. Girgrah values personal connections and the best interests of the physician group, as well as all employees,” says Francis Rodwig, Jr., MD, medical director of Professional Staff Services and medical director of Transfusion Medicine at Ochsner. “He is authentic in his relationships and he models the behavior of an emotionally intelligent leader.”
Executive Vice President and Chief Medical Officer at Ochsner, Robert Hart, MD, echoes Dr. Rodwig’s sentiments.
“When we started the task force, it was very clear that he had a passion for this. If you spend much time with him, he has a very compassionate side,” says Dr. Hart.
Dr. Girgrah was not always leading the charge against physician burnout. His medical journey started in Toronto where he completed his MD and PhD, but it was his “midlife crisis” that led him to New Orleans in 2007 where he was attracted to the culture, environment and community.
“I came to interview here nine months after Katrina. At the time, I wasn’t really looking to leave Toronto, but I was curious. I remember my father had once told me that it was his favorite American city,” he says, adding that he was drawn to the hospital’s culture, and the vibe of the city and community.
It wasn’t until 2013 at his 20-year medical school reunion, though, that he stumbled into an interest in physician burnout and well-being.
“I found out some alarming things about a couple of my med school colleagues having exited the profession in one way or another,” says Dr. Girgrah. “I probably hadn’t heard of burnout before, but that’s when I started reading about it.”
With profound interest in learning more, his adjusted course led him down a new path toward chief wellness officer.
Identifying the source of the problem
Physicians often think they can do everything, but if they cannot do something they often blame themselves. He wants to send a message to physicians that “this is primarily a systems issue and that it’s not their fault.”
“The few times burnout had been talked about, it always seemed to be talked about after a conversation about patient experience or after a conversation about quality and safety,” Dr. Girgrah says, adding that he always felt when burnout was discussed after these conversations, it “elicited some degree of cynicism, particularly on the part of the frontline physicians.”
Instead of talking about burnout as the right thing to do, it was always just a means to an end. However, by addressing it, he believes other very important things around compassionate care, patient experience, quality and safety, discretionary effort, and financial performance will follow.
Because Ochsner did not know much about burnout, they began by surveying the group practice to understand the problem before finding a solution.
“It was clearly a problem growing around the country and we recognized we were not immune from it,” says Dr. Hart. “I’ve been in health care as a physician for 30 years and clearly the demands have become greater. There are a lot of demands from physicians that has created this burnout and we recognized that among our own staff.”
“We did the math with a survey a little over a year ago and we were a little bit better than the average across the country, but clearly it was something that we had to address for our physicians and advanced practice providers (APPs), as well as for our patients,” adds Dr. Hart.
The Maslach Burnout Inventory was completed in August 2017 drawing from about 800 respondents. While Maslach was considered the industry standard at the time, Dr. Girgrah felt it was a cumbersome tool that required them to “go through it with a fine-tooth comb to get any sort of demographic data.”
This survey highlights three primary dimensions of burnout—depersonalization, lack of personal accomplishment and emotional exhaustion. It also describes six dimensions in work-life centered around sense of community, values, control, rewards, reward recognition, fairness and workload.
“We were doing reasonably well against national benchmarking in describing lack of depersonalization, a greater sense of personal accomplishment, a sense of community in the workplace and congruence of personal with organizational values,” says Dr. Girgrah.
However, Ochsner was doing relatively poor in “describing more emotional exhaustion, sense of lack of control with a work environment, not being rewarded or recognized, and a fair and manageable workload.”
After carefully looking at physician engagement surveys, he conducted three months of focus groups to begin taking the right steps toward improving organizational well-being. During his visits to different campuses with a variety of groups of physicians, he asked doctors what went into a good day at work, but also tackled what made for a bad day.
“We always seem to talk about burnout as being binary—present or absent. The surveys report back on the percentages of burnout, but clearly, it’s fluid, it operates along a continuum, even within an individual and within departments,” says Dr. Girgrah.
While Dr. Girgrah was happy to see that Ochsner was not worse than the national average, there were five areas of opportunity with the first being respecting a physician’s time. To the extent possible, physicians want to spend more time with their patients or families. However, they also want to spend less time doing what is perceived as “menial rather than meaningful interactions,” such as clerical work.
The second theme in some departments—particularly for surgeons—was centered around having the fundamental tools to care for patients.
Some surgeons found inconsistencies in the availability of tools needed for proper care. If they don’t have the right tools or environment to perform their daily duties, it makes being a surgeon more difficult. Knowing this, Dr. Girgrah wants to make sure they can escalate the problem and get what they need.
The third area, that was not consistent throughout the organization, was around building the team.
“Not just physicians and APPs, but everybody that interacts with the patient along the care continuum, so medical assistants, nurses, PharmDs,” he says. “There were variations in departments who had mature, highly functioning nurses and medical assistants who had been with their team for a long period of time. It was like, ‘what’s burnout?’
“Then you’d have a department that had rapid turnover of medical assistants, poorly defined scope of practice as medical assistants and nurses. Those departments were hurting,” Dr. Girgrah adds.
“A fourth theme would have been around conflicting priorities,” he says. “One month let’s focus and double down on patient access and then next month, let’s double down on financial production.”
“We all recognize that health care is really complicated and there are many priorities, but from a level of the frontline physician, to the extent possible, they want us to focus what we’re saying the priorities are,” says Dr. Girgrah. “Make it go down from 30 things on their dashboard to three things. Leaders will always be accountable for 30 different things, but I think our frontline folks need to have things simplified.”
The last theme centered around messaging because “there seems to be a desire to have more progress improvement messaging and positive messaging, not just results,” he says.
This plays into the competitive value in New Orleans. “Addressing burnout is the right thing to do,” says Dr. Girgrah, adding that “our group practice is our secret sauce and addressing physician well-being gives us a competitive advantage.”
Designing the proper solutions
New surveys will be distributed soon, allowing Dr. Girgrah to begin creating and developing solutions to address burnout. Yet, he is getting increasingly impatient because he wants to start implementing interventions to take steps toward an improved workforce.
“I’m a pretty analytical person, but honestly it’s very hard to read a descriptive article about burnout—they all are starting to sound the same. I’m just interested now in moving on to solutions,” says Dr. Girgrah. “I definitely think personal resilience will be important, but I don’t think that’s the first thing we want to offer our providers.”
“The heavy lifting is going to be around practice efficiency and there is a thirst to hear what we can do tomorrow to make their lives easier,” he adds.
Dr. Hart adds that Ochsner was “concerned about unveiling a program too early since there have been initiatives in the past that never gained any traction. Now that the office has started, we have provided extra communication to them about our timeline.”
“The two most important areas to address first are optimization of the electronic medical record and working with our administrative partners to identify and eliminate any tasks that do not provide any value,” Dr. Hart says.
“Historically, we’ve been working downstream and being very reactive, working on the coping mechanisms, dealing with crises, but we need to get upstream,” Dr. Girgrah says. “We need to either decrease the frequency or the severity of stressors and increase recovery time, or decrease exposure to those stressors where we’re going to acknowledge that there’s always going to be stressors in the work environment.”
Another area that is key to success is establishing a connection with physicians and other health care team members at Ochsner. Without their support, the goals will be unattainable—something Dr. Girgrah does not want.
For him, that begins with his credibility as a physician and knowing what doctors are going through.
If he had to break down his job description, it would be 50% chief wellness officer, 30% medical director and 40% patient care. While he is aware that adds up to 120%, he says he would have a hard time giving up patient care because it brings him so much joy.
“I also fear I would have a credibility issue if I wasn’t seeing patients, so it’d be very hard for me to discuss burnout and discuss the interventions with frontline providers if they didn’t feel that I was in it with them, sort of seeing patients, understanding what it’s like,” adds Dr. Girgrah.
Defining the right metrics for success
“Clearly this isn’t going to be a journey where success is managed and measured in weeks or months. This is a cultural journey over three to five years,” Dr. Girgrah says. “That’s not to diminish that there don’t need to be quick wins, but this isn’t going to be solved by the end of the year.”
Executives and doctors at Ochsner are looking for improvements measured through physician engagement and burnout scores assessed by the Mini Z survey, as well as decreased turnover.
Since distributing the Mini Z burnout survey in collaboration with the AMA, physicians and advanced practice providers have said it is “much easier to complete than the Maslach burnout inventory that went out two years ago,” says Dr. Girgrah. “Feedback from our physicians and APPs has been very receptive.”
“The first day it went live, we heard back that we had the most responses from any health system,” he says.
However, in the short term, Dr. Girgrah knows there needs to be action around secondary metrics, such as “work after work.”
“I need to show my physicians, as well as my executive team, that we are earnest in our efforts to decrease that work after work,” he says.
When looking at the 100 most struggling physicians in Epic out of just under 1,400 doctors, they are spending an average of 90 minutes in the EHR after hours. We’re also looking at the data with our APPs.
Of course, Dr. Girgrah might not be able to eliminate the after-hour work completely, but he needs to ensure it does not get worse and start shaving off time—whether that is accomplished through Epic badge log-in, pharmacy refills or decreasing in-basket messaging.
“One thing we are doing immediately is looking at those 100 most struggling physicians and providing them immediate help with Epic retraining and not penalizing them for that,” he explains. “Giving them four hours of customized retraining in Epic and making sure that they’re not being penalized for work being missed in terms of income—that’s priority one.”
The other idea is that those 100 physicians may not be struggling because they are not proficient in the EHR. Instead, it is because even the most proficient doctor might just have too much work. By looking at the data, Dr. Girgrah can see if they can delegate work and why those doctors are spending extra hours after work.
Historically the business case around creating efficiency interventions—whether it is giving 30 minutes back to the physician through Epic badge log-in or giving a full 40 minutes back to the doctor by helping with the in-basket—has always been, “OK, how many more patients can they see with that time?”
“Now the business case is, ‘Wow, that’s a great thing to do.’ And whether they choose to spend more time with their family, that’s up to the physician,” says Dr. Girgrah. “It's finding a balance between fixing that work after work and then maybe also still offering some sort of resiliency training or outside sources for that.”
“The last thing I think a burned-out physician wants to hear is me promoting a yoga class or meditation class right away. They may eventually benefit from that, but what they need in the short term is an hour back to their day and how that is done, that’s the $64,000 question. I’m not diminishing the importance of personal resilience, but I just feel that can’t be what they hear first,” he says.
For example, physicians are sometimes asked to attend extracurricular meetings from five to six in the evening. To address that this takes away from time at home, Ochsner is working on the creation of a program to send those physicians home with a meal, not just for themselves, but for their family.
“It sends a message to the family that this organization values your husband’s time, your wife's time, your father's time because we asked him to stay an extra hour. Why not put your money where your mouth is and show physicians?” says Dr. Girgrah, adding that “they may sound like not very significant things, but I think these acts do send messages both to the physicians and to their families.”
“We are tackling this because it’s an organizational and professional imperative and it’s the right thing to do, not because we’re worried about our economic future or other things,” he says. “We are doing this because it is the humanitarian and compassionate thing that the group practice in an organization does for its physicians.”
Incorporating the Mini Z survey
To combat physician burnout, health systems and organizations need to identify stress in its earlier stages. These organizations also need to choose programs to prevent burnout before it occurs. With the 10-item Zero Burnout Program survey, also known as the Mini Z, organizations can identify burnout, stress and potential solutions.
The Mini Z survey is short and easy to use, and should be distributed annually to all physicians in your health system. Physicians can access the burnout survey online via their computers, smartphones or other devices.
Nigel Girgrah, MD, has partnered with the AMA to distribute the Mini Z burnout survey to physicians at Ochsner. He plans to use the survey to continue to address the needs of physicians at Ochsner because it only took him eight minutes to complete on his smartphone. He believes it will provide higher response rates due to the ease of completion while “in department meetings because everybody has their smartphone with them.”
“I love the fact that it will provide a more easily accessible demographic data than the Maslach Burnout Inventory,” Dr. Girgrah says. “It should allow us to benchmark against other organizations and consider departments from Ochsner with two similar departments at other health systems.”
Once the physicians have completed the burnout survey, the Mini Z data should be shared with practice leaders or office staff. An easy way to share Mini Z survey results is by creating a document with summary data for all respondents. After reviewing the data, it is important to identify the areas of greatest concern—either practice- or organization-wide, or by department. Based on the problem areas identified, select appropriate interventions to address them.
“What’s more exciting for me is it allows us to actually test interventions. You can use the Mini Z to pre-select those folks that you’re going to be testing an intervention on to see whether it makes any difference,” says Dr. Girgrah.