Pharmacy Benefit Managers under scrutiny
The AMA is putting Pharmacy Benefit Managers (PBM) in the hot seat this week, as it released a new AMA analysis on PBMs and endorsed newly introduced legislation that would bring long-overdue transparency, accountability and fairness to the PBM industry.
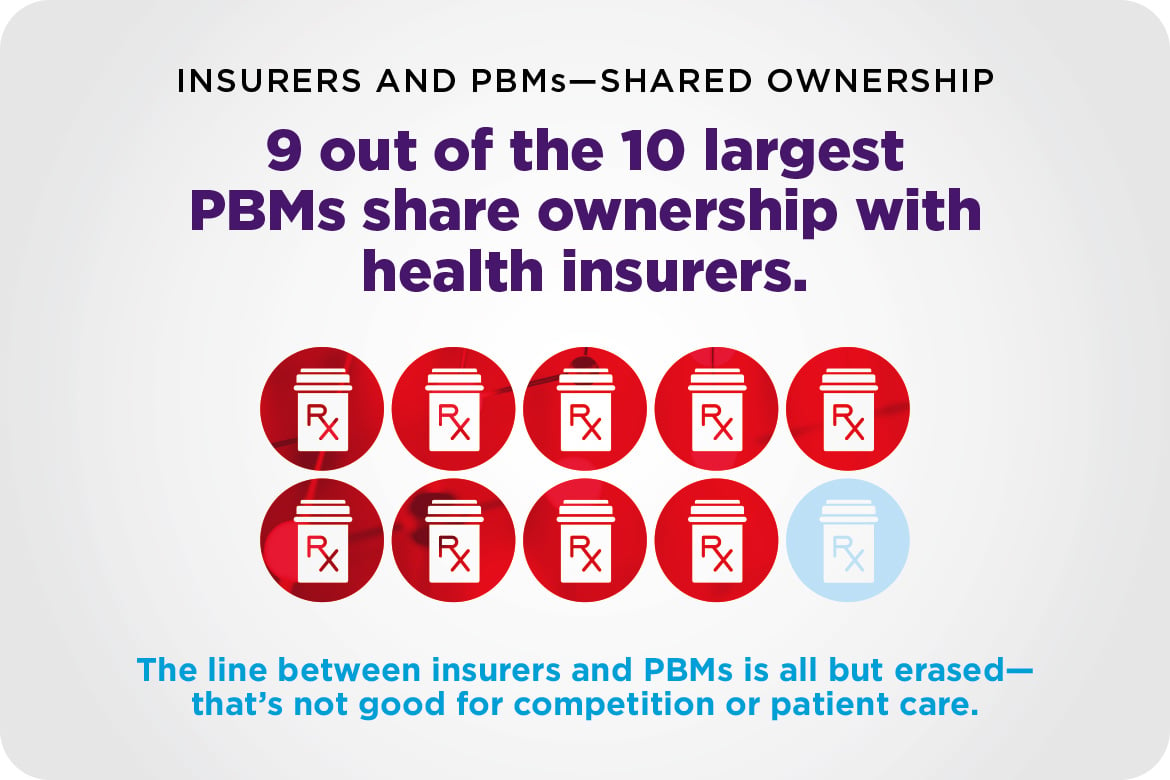
PBM markets are at risk of harming patients
A new AMA analysis demonstrates low competition in PBM markets across the nation and high vertical integration as the largest PBMs share ownership with health insurers. This analysis adds to growing concern over anticompetitive harm resulting from low competition and high vertical integration in the PBM industry.
Bipartisan legislation would rein in PBM abuses
The AMA formally endorsed (PDF) H.R. 4317, the “Pharmacy Benefit Manager (PBM) Reform Act of 2025,” introduced by Representatives Earl “Buddy” Carter (R-GA) and Debbie Dingell (D-MI). This bipartisan legislation seeks to bring long-overdue transparency, accountability and fairness to the PBM industry, an increasingly powerful force in the prescription drug supply chain.
The PBM Reform Act would ban spread pricing in Medicaid, establish a transparent reimbursement model to ensure pharmacies are fairly compensated, decouple PBM compensation from drug prices, increase disclosure to employers and patients, and authorize the U.S. Department of Health and Human Services to enforce fair contract terms.
Physicians have long raised concerns about the lack of clarity around formulary placement, utilization requirements such as step therapy, and patient cost-sharing obligations, all of which are heavily influenced by PBMs and often hidden from both prescribers and patients. A recent AMA analysis of competition in PBM markets (PDF) further highlights how vertical integration and market concentration threaten access and affordability.
The AMA commends Representatives Carter and Dingell for their leadership and remains committed to working with Congress to ensure prescription drugs are affordable, accessible and guided by medical expertise, not opaque corporate negotiations. H.R. 4317 was introduced on July 10 and currently has 21 cosponsors.
More articles in this issue
- Aug. 1, 2025: Medicare Payment Reform Advocacy Update
- Aug. 1, 2025: National Advocacy Update
- Aug. 1, 2025: State Advocacy Update