What are PBMs and what do they do?
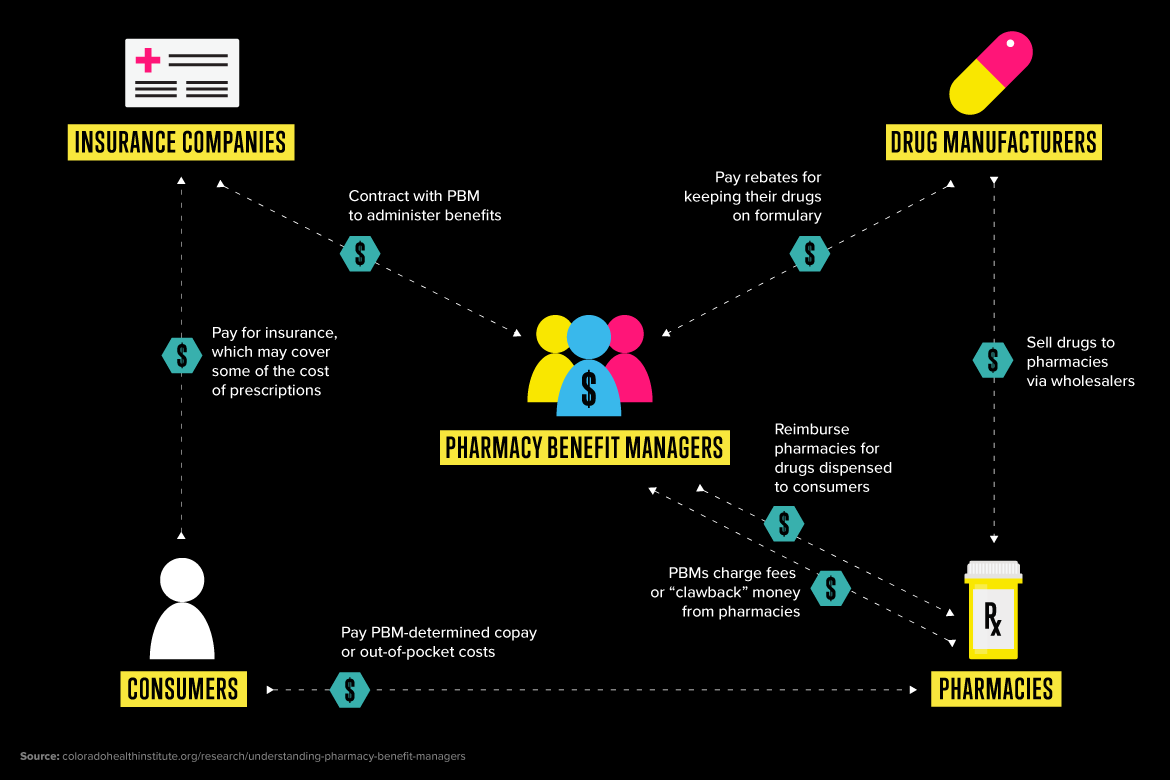
Pharmacy benefit managers (PBMs) manage prescription drug plan (PDP) benefits for insurers and/or employers. PBMs are “middlemen” in the prescription drug supply chain. PBMs were established in the 1960s to help insurers control prescription drug spending and manage benefits. Consolidation and vertical integration in the PBM market have raised concerns about the potential for reduced competition and higher prescription drug prices.
Their primary functions include:
- Negotiating rebates and discounts with drug manufacturers
- Managing drug formularies
- Assembling retail pharmacy networks
- Processing and adjudicating pharmacy claims
- Designing drug benefits
- Conducting utilization management (e.g., prior authorization, step therapy)
Learn more about PBMs and their role in drug pricing at TruthinRX.
Why can PBMs be controversial?
While PBMs can help control drug spending, they can also lessen competition. Low competition can lead to:
- High prices paid by insurers for PBM services.
- Incomplete rebate pass-through: Negotiated rebates may not fully passed through to consumers.
- Higher insurance premiums.
- Lower reimbursement to pharmacies.
In addition, high vertical integration of insurers and PBMs can lead to non-affiliated insurers losing access to PBMs.
What is the AMA doing about PBMs?
Conducting research
An AMA study titled Competition in PBM Markets and Vertical Integration of Insurers with PBMs: 2025 Update (PDF) presents an analysis of PBM markets and the provision of PBM products to insurers. It reports the 10 largest PBMs and drug insurers in the U.S. and summarizes concentration levels (HHIs) in those PDP region-level markets. The study finds low competition in PBM markets and high vertical integration of insurers with PBMs.
Key findings include:
- The four largest PBMs collectively had a 67% share of the national PBM market in 2023.
- Seventy-nine percent of PDP region-level PBM markets lacked adequate competition and were “highly concentrated” according to 2023 federal antitrust guidelines (PDF).
- At the national level, 77% of commercial and Part D enrollees were in a prescription drug plan (PDP) where the insurer and PBM were vertically integrated.
Advocacy
- 8 wins for doctors, patients in latest federal budget deal: Targeted pharmacy benefit manager (PBM) reforms introduced to enhance transparency, curb abusive Medicare drug rebate practices, and strengthen enforcement against anticompetitive behavior. These provisions represent tangible progress toward lowering prescription-drug costs and improving fairness in the drug supply chain for patients and physicians. Learn more with this Leadership Viewpoints column, “Unchecked power in PBM industry puts patients at risk of harm,” by AMA President Bobby Mukkamala, MD.
- Stay current with PBM reform by visiting TruthinRX, an AMA grassroots advocacy campaign. This campaign explores common PBM practices, current events, and patient stories related to drug price transparency.
Supporting PBM reform
The AMA wrote a letter to Congressional sponsors in support of the Pharmacy Benefit Manager Reform Act of 2025 (HR 4317) (PDF).
Council on Medical Service reports
- CMS Report 5-A-19: The Impact of Pharmacy Benefit Managers on Patients and Physicians (PDF)
- CMS Report 05-A-23: Prescription Drug Dispensing Policies (PDF)
- Report 6-A-24: Economics of Prescription Medication Prior Authorization (PDF)
- CMS Report 6-A-25: Prescription Medication Price Negotiation (PDF)
Policy briefs
- Prescription Drug Pricing & Cost Transparency (PDF)
- Mandatory White Bagging and Brown Bagging Policies Threaten Patient Access to Care (PDF)
As PBMs increasingly act in their own self-interest without transparency or accountability, drug prices rise and patients face health risks from cost-prohibitive drug treatments. The AMA’s analysis is intended to provide insight to help policymakers understand the anticompetitive conditions in the PBM market that can result in harm to patients. The AMA fully supports greater transparency and accountability that is needed to prohibit PBMs from engaging in opaque and harmful business practices.
—AMA President Bobby Mukkamala, MD, on the harm of PBM markets for patients.
Explore other AMA resources on PBM reform
- Competition in health care research
- JAMA Health Forum™: Pharmacy Benefit Managers: History, Business Practices, Economics, and Policy
- AMA Ed Hub™: The History, Economics, and Policy Context of Pharmacy Benefit Managers
- JAMA Health Forum™: Use of and Steering to Pharmacies Owned by Insurers and Pharmacy Benefit Managers in Medicare