As more people are vaccinated against COVID-19 and communities further reopen, a key question remains: How will—and how should—health care change after the pandemic ends? During a Saturday plenary session of the June 2021 AMA Section Meetings, AMA member Shantanu Nundy, MD, shared a framework for what health care advocacy, equity, innovation and outcomes should look like in a post-pandemic world.
“COVID has been an incredible magnifying glass on the core challenges of health care,” said Dr. Nundy, an internist in the greater Washington, D.C, area. He is also the chief medical officer of Accolade, a personalized health and benefits solution for employers, health plans and their members headquartered in Plymouth Meeting, Pennsylvania.
“We’ve been seeing health inequities our entire career but seeing those charts on the front page of the New York Times with three times the death rate in African Americans—that has created a real moment now where people are saying this is not acceptable,” he said. Dr. Nundy previously served as director of the Human Diagnosis Project, a health care AI startup company, and managing director for clinical innovation at Evolent Health, a population health and predictive analytics company, where he improved hospital and chronic disease outcomes for more than 2 million individuals in the U.S.
Dr. Nundy outlines a framework for post-pandemic health care and the central role of the physician in leading change in his book, Care After COVID: What the Pandemic Revealed Is Broken in Healthcare and How to Reinvent It.
Care must be distributed
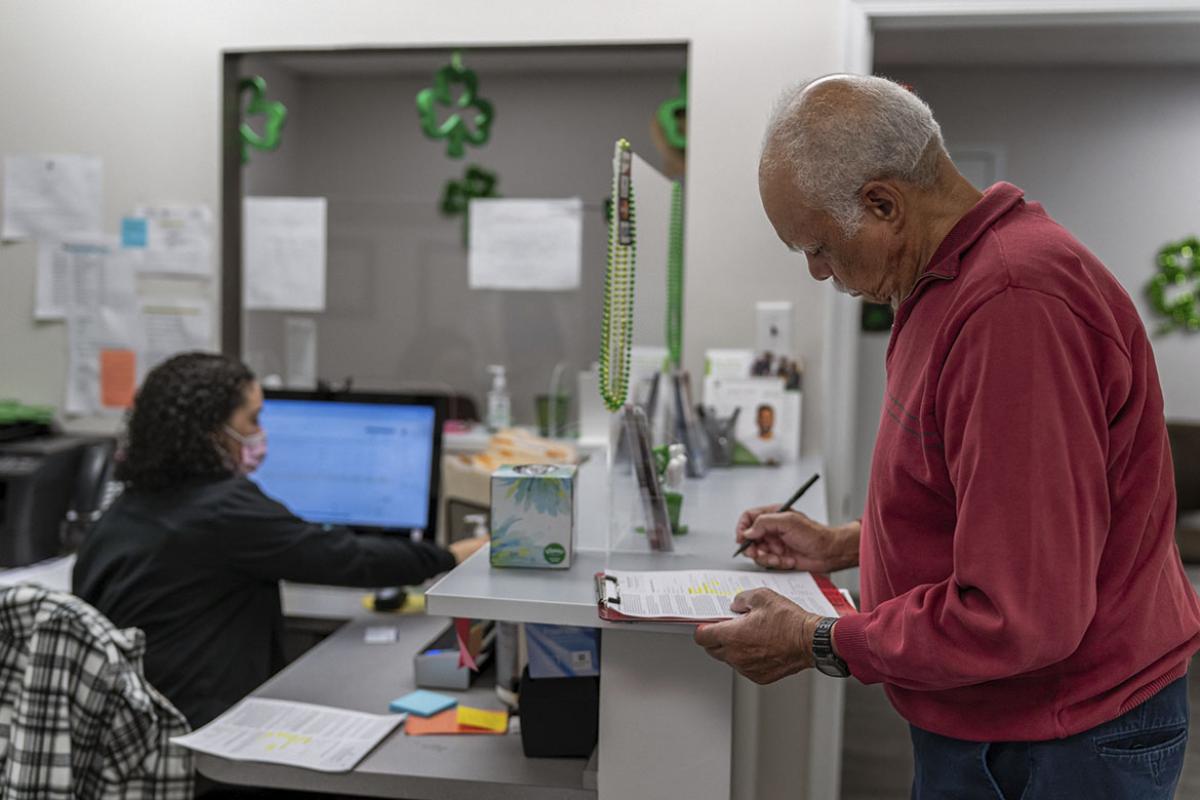
“Care needs to happen where health happens, which starts in the home and in our communities,” Dr. Nundy said.
For example, “very often now we’re talking about ‘virtual,’ we’re talking about ‘home-based,’ but that misses the bigger picture,” he said. “Distributed is a more inclusive, broader term that says: Look, virtual and home is one part of the health care experience … and we need all of those parts working together in concert ultimately to serve our patients.”
Watch this episode of the “AMA COVID-19 Update” in which Dr. Nundy shared his post-pandemic patient focused framework.
Ensure care is digitally enabled
“The real role for technology in health care is to increase relationships in health care, which are central, and particularly trust,” Dr. Nundy said.
For example, when practicing in Chicago, Dr. Nundy noticed a lot of his patients had a hard time making it to appointments, taking their medications and learning about their conditions, but were always staying connected to each other using texting. That’s when he decided to build a text message-based system to help people with their chronic conditions.
“That worked for people who did have phones and did have emails, but it also worked for those who didn’t,” he said.
Decentralize resources for care
“We need to put way more resources in the hands of front-line teams—as well as patients—to enable them to make better care decisions for themselves,” Dr. Nundy said. A “physician-led world that will serve patients best,” he added.
For example, one of Dr. Nundy’s patients was in and out of the hospital with heart failure. With heart failure, patients need to check their weight every day, Dr. Nundy explained. But when he found that his patient didn’t have a weighing machine because she could not afford it, he looked in his office.
When he found none, Dr. Nundy reached into his pocket, handed his patient $20 out of his wallet and she didn’t get admitted to the hospital again.
This represents decentralized care because, “why couldn’t I have given her a weighing scale?” Dr. Nundy said, adding that it’s about “putting the resources into the doctors and care teams who understand what the patients need.”
Doctors must play central role
“As physicians, we have this incredible privilege of really understanding our patients and really having an understanding of the evidence and outcomes, as well as we really have the trust and respect of our colleagues,” Dr. Nundy said.
“What I've learned in my career is that when you're doing the same thing or something incremental, you may or may not need a physician at the helm. But when you're actually advocating for a completely different way of doing it, everyone in the room’s looking to you to say that this is the right direction to go,” he added.
Make innovation work for all patients
“What’s been true for a long time, but again has only been magnified during the pandemic, is that innovation and equity must be synonymous,” said Dr. Nundy, one of 11 external advisers for the AMA’s strategic plan to embed racial justice and advance health equity.
“We can’t look at it as an afterthought,” said Dr. Nundy. “When we build solutions, it must work for the people who are most vulnerable rather than trying to take a solution that works for the median patient and then somehow retroactively apply it.”
This plenary session also included a panel discussion hosted by AMA Chief Experience Officer and Senior Vice President Todd Unger. The panel included:
- Todd Askew, AMA senior vice president of advocacy.
- Meg Barron, AMA vice president of Digital Health Innovations.
- Karen Kmetik, PhD, AMA group vice president of Health Outcomes.
- Aletha Maybank, MD, MPH, AMA chief health equity officer and senior vice president.
The panelists explored topics such as what health care advocacy, equity, innovation and outcomes will look like in a post-pandemic world.
The AMA has developed a COVID-19 resource center as well as a physician’s guide to COVID-19 to give doctors a comprehensive place to find the latest resources and updates from the CDC and the World Health Organization.