If you’re preparing for the United States Medical Licensing Examination® (USMLE®) Step 1 exam, you might want to know which questions are most often missed by test-prep takers. Check out this example from Kaplan Medical, and read an expert explanation of the answer. Also check out all posts in this series.
The AMA and Kaplan have teamed up to support you in reaching your goal of passing the USMLE® or COMLEX-USA®. If you're looking for additional resources, Kaplan provides free access to tools for pre-clinical studies, including Kaplan’s Lecture Notes series, Integrated Vignettes, Shelf Prep and more.
This month’s stumper
A 60-year-old man comes to the physician because of a constant cough that keeps him awake at night. He denies sputum production, fevers, or chills. He has a history of type 2 diabetes mellitus, hypertension, hypercholesterolemia, asthma, and heart failure. He is currently taking albuterol, theophylline, atorvastatin, metoprolol, enalapril, hydralazine and digoxin.
Replacement of one of this patient's current medications with which of the following drugs will most likely improve his symptoms?
A. Atenolol.
B. Diltiazem.
C. Exenatide.
D. Glimepiride.
E. Losartan.
F. Propranolol.
G. Sitagliptin.
The correct answer is E.
Kaplan Medical explains why
The key to answering this question is identifying the current treatment associated with a chronic, nonproductive cough. Then you should determine which of the answer choices has a similar mechanism of action to the causative agent.
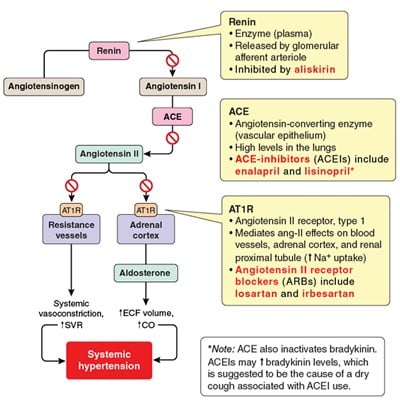
The lack of a fever or sputum production suggests that the patient's coughing is not caused by a pathogen. Coughing does occur in a small percentage of patients using an angiotensin-converting enzyme (ACE) inhibitor (e.g., enalapril, lisinopril) however. ACE converts angiotensin I to angiotensin II (ang-II), but it also inactivates bradykinin. ACE inhibitors are used in the treatment of hypertension because they block ang-II formation, but they also impair bradykinin metabolism. Bradykinin accumulation is suggested to cause the dry cough.
The physician should replace the ACE inhibitor with an ang-II receptor antagonist (ARB) such as losartan, which is an alternative therapy for hypertension. ARBs block the same pathway as ACE inhibitors (i.e., the renin-angiotensin-aldosterone system; RAAS) but have a lower incidence of chronic cough because they do not interfere with bradykinin metabolism. Losartan use is associated with hypotension, hyperkalemia, and angioedema.
Why the other answers are wrong
Choice A and F: Atenolol is a beta-1 selective antagonist. Propranolol is a nonselective beta antagonist that is associated with respiratory difficulties if administered to patients with asthma or chronic obstructive pulmonary disease (COPD). These agents are known to cause bradycardia, heart block, Raynaud phenomenon, and bronchospasm in asthmatic patients.
Choice B: Diltiazem is a calcium channel blocker used in the treatment of hypertension and cardiac dysrhythmias. Bradycardia and negative inotropic effects are commonly associated with the use of this agent. Therefore, this drug would not be recommended for use in a patient with heart failure.
Choice C: Exenatide is glucagon-like-peptide (GLP-1) receptor agonist indicated for the treatment of type 2 diabetes. It is most commonly associated with hypoglycemia, especially if administered with a sulfonylurea.
Choice D: Glimepiride is a sulfonylurea indicated for the treatment of type 2 diabetes and is commonly associated with hypoglycemia.
Choice G: Sitagliptin is an orally active inhibitor of the dipeptidyl peptidase-4 (DPP-4) and is indicated for the treatment of type 2 diabetes. It is most commonly associated with hypoglycemia, especially when administered with other oral hypoglycemic agents.
Tips to remember
- ACE inhibitors can cause a dry cough by blocking bradykinin metabolism.
- Losartan, an angiotensin II receptor antagonist, has similar therapeutic effects as ACE inhibitors but has a much lower incidence of cough.
- Switching from an ACE inhibitor to an angiotensin II receptor antagonist is generally effective in alleviating the chronic cough.
For more prep questions on USMLE Steps 1, 2 and 3, view other posts in this series.