Contents
- AMA urges prior authorization reform
- Prior authorization toll exceeds alleged benefits, say physicians
- AMA comments support CMS’ work on prior authorization
- AMA comments on CMS proposed rule on electronic attachment standards
- AMA survey data in the news
- More articles in this issue
- Essential Tools & Resources
More than four in five physicians report that prior authorization requirements led to higher overall utilization of health care resources: AMA urges reform
New AMA survey results illustrate a critical need to streamline the prior authorization process and eliminate low-value requirements to minimize waste, delays, and disruptions in care delivery. The AMA has taken a leading role in advocating for prior authorization reforms and submitted comments to the Centers for Medicare & Medicaid Service (CMS) largely supporting the agency’s proposals to improve prior authorization. Learn more about the survey results and highlights of these comment letters.
Toll from prior authorization exceeds alleged benefits, say physicians
The approval process health insurers impose on medical services or drugs is generating a toll that exceeds the purported benefits, according to a recent physician survey released by the AMA and shared in a letter to federal health officials. While health insurers claim prior authorization requirements are used for cost and quality control, a vast majority of physicians say authorization controls lead to unnecessary waste and avoidable patient harm.
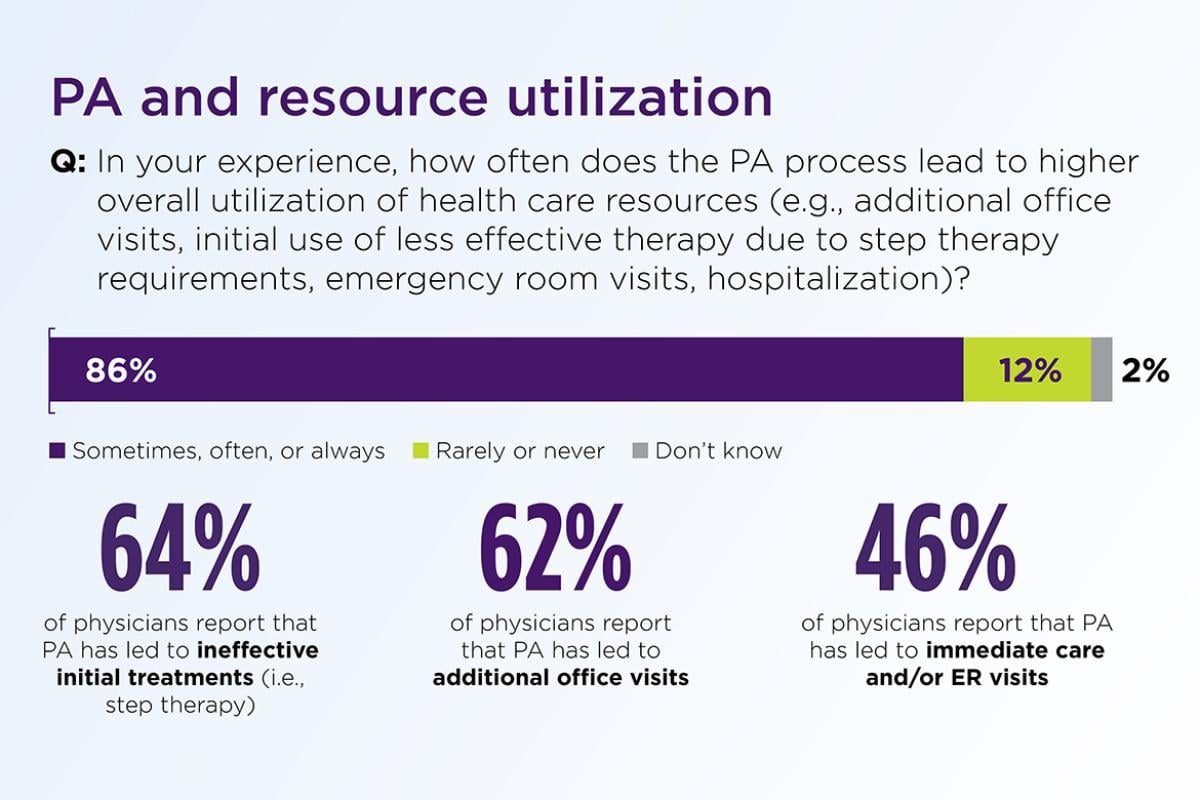
According to the AMA survey, more than four in five physicians (86%) reported that prior authorization requirements led to higher overall utilization of health care resources, resulting in unnecessary waste rather than cost-savings. More specifically, about two-thirds of physicians reported resources were diverted to ineffective initial treatments (64%) or additional office visits (62%) due to prior authorization policies, while almost half of physicians (46%) reported prior authorization policies led to urgent or emergency care for patients.
The health insurance industry maintains prior authorization criteria reflect evidence-based medicine, but physician experiences call into question the clinical validity of insurer-created criteria that lack transparency. Only 15% of physicians reported that prior authorization criteria were often or always evidence-based.
Other critical concerns highlighted in the AMA survey include:
Patient Harm: One-third of physicians (33%) reported that prior authorization led to a serious adverse event for a patient in their care, including hospitalization, permanent impairment, or death.
Bad Outcomes: Nearly nine in 10 physicians (89%) reported that prior authorization had a negative impact on patient clinical outcomes.
Delayed Care: More than nine in 10 physicians (94%) reported that prior authorization delayed access to necessary care.
Disrupted Care: Four in five physicians (80%) said patients abandoned treatment due to authorization struggles with health insurers.
Lost Workforce Productivity: More than half of physicians (58%) who cared for patients in the workforce reported that prior authorizations had impeded a patient’s job performance.
In addition, a significant majority of physicians (88%) said burdens associated with prior authorization were high or extremely high. This costly administrative burden pulls resources from direct patient care as medical practices complete an average of 45 prior authorizations per physician, per week, which consume the equivalent of almost two business days (14 hours) of physician and staff time. To keep up with the administrative burden, nearly two in five physicians (35%) employed staff members to work exclusively on tasks associated with prior authorization.
The AMA continues to work on every front to streamline prior authorization. Through the AMA Recovery Plan for America’s Physicians the AMA is working to right-size prior authorization programs so that physicians can focus on patients rather than paperwork. For more information, read the full press release or view the complete survey results.
AMA public comments support CMS’ work on prior authorization and interoperability
The AMA submitted public comments on March 13 to the Centers for Medicare & Medicaid Services (CMS) on the Notice of Proposed Rulemaking to advance interoperability and improve prior authorization (PA). Overall, with its December 2022 Physician Survey results, the AMA supported CMS’ steps to support judicious, transparent and clinically appropriate use of PA that protects patients’ access to treatment. In addition, the AMA encouraged efforts to increase patient access to their medical information through health plan-enabled and maintained application programing interfaces (APIs). The AMA also urged CMS to consider how its policies can better strengthen patients’ data privacy while limiting physician burden.
In terms of Medicare Advantage (MA) Plans, the AMA comments strongly supported their inclusion in the scope of this rule but urged CMS to leverage a regulatory pathway that will apply to all health plans when mandating PA-related implementation guides and transaction standards in any future rulemaking. The AMA also encouraged CMS to further explore the need to designate an electronic transaction standard for drugs covered under a medical benefit and recommended that CMS strengthen the requirement for health plans to provide a specific reason for a PA denial to ensure that the information is understandable and outlines clear, actionable next steps. While commending CMS for the patient-centric focus of this regulation, the AMA did also recommend that CMS shorten the required PA processing timeframes to 48 hours for standard PAs and 24 hours for expedited PAs to protect patient safety. However, the AMA opposes any efforts to link PA reform to physicians’ success in CMS’ Quality Payment Program. The AMA urged CMS to explore alternatives to promote physician uptake of electronic PA.
The March 13 letter also supported CMS’ requirements on health plans to exchange data with physicians using APIs and asked CMS to consider how its health plan API requirements align with 21st Century Cures Act requirements around information sharing.
AMA also comments on CMS proposed rule on electronic attachment standards
The AMA also recently submitted separate comments in response to a proposed rule issued by CMS regarding transaction standards for electronic attachments, which would support the exchange of clinical documentation between physician practices and health plans. The AMA expressed appreciation for the underlying intention of CMS’ proposals to streamline prior authorization (PA) and support administrative simplification, as fixing PA constitutes a key pillar in the AMA’s Recovery Plan for America’s Physicians.
However, the AMA urged CMS to postpone adoption of any standards for PA attachments because recent technology and regulatory developments have significantly altered the electronic PA transaction landscape and warrant further study prior to mandating attachment standards for this purpose. In contrast, the AMA argued that claim attachments represent a separate and distinct use case that is ripe for automation via the proposed standards. As such, the AMA recommended that CMS finalize its proposals related to claim attachment standards as written to reduce administrative burdens and costs across the health care industry.
AMA survey data in the news
Results of the new AMA prior authorization survey are making an impact on Capitol Hill and in the news. Recent highlights include:
- Op-ed in the Washington Examiner from Rep. Larry Bucshon (R-IN): “It’s time to get Washington out of the doctor’s office”
- “That is why I and several of my colleagues introduced the Improving Seniors’ Timely Access to Care Act, a bill that would ensure coverage decisions for Medicare Advantage patients are made quickly and effectively. According to a recent study by the American Medical Association, 24% of physicians have reported that delays in the prior authorization process have led to a patient getting hospitalized. This is unacceptable. Patients must not be forced to wait days, weeks, or even months to know whether care prescribed by their doctor will be covered by insurance.”
- Social media posts from Rep. Suzan DelBene (D-WA) saying “Nearly 9 in 10 physicians report that insurance red tape has a negative impact on patient clinical outcomes.” (Twitter, Facebook)
- Video and story on Investigate TV highlighting survey data: “Permission to Practice: Doctors, patients say insurance prior-authorizations put profits over people”
More articles in this issue
Table of Contents
- More than four in five physicians report that prior authorization requirements led to higher overall utilization of health care resources: AMA urges reform
- Toll from prior authorization exceeds alleged benefits, say physicians
- AMA public comments support CMS’ work on prior authorization and interoperability
- AMA also comments on CMS proposed rule on electronic attachment standards
- AMA survey data in the news
- More articles in this issue