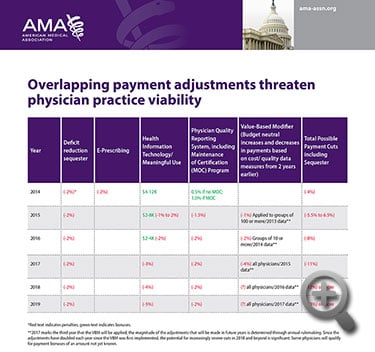
Physicians providing care to Medicare patients could face a “tsunami” of regulatory penalties over the next 10 years, potentially seeing payments cut by more than 13 percent by the end of the decade. The AMA urged the Centers for Medicare & Medicaid Services (CMS) to streamline the competing laws and regulations that threaten access to care in a letter (PDF) sent Tuesday.
Next year, some physicians could face cuts of more than 6 percent under the Medicare sequester cut and penalties from overlapping regulatory programs, including the meaningful use electronic health record (EHR) program, the Physician Quality Reporting System (PQRS) and the Value-Based Modifier program (VBM).
“Physicians want to provide our patients with the best care possible, but today there are confusing, misaligned and burdensome regulatory programs that take away critical time physicians could be spending to provide high quality care for their patients,” AMA President Robert M. Wah, MD, said in a news release. “Government leaders should take the necessary steps to eliminate this regulatory nightmare and ensure America’s seniors can continue to receive the high-quality care they deserve.”
The AMA told CMS these programs make it difficult for physicians to invest in health IT and payment and delivery reforms necessary to improve patient care. The AMA urged CMS to simplify and align incentive programs to ensure there is one streamlined process in place for physicians to meet a single set of quality reporting requirements, rather than the three separate sets of requirements that currently exist.
“No other segment of the health care industry faces penalties as steep as these, and no other segment faces such challenging implementation logistics,” the letter said. “The tsunami of rules and policies surrounding the penalties are in a constant state of flux due to scheduled phase-ins and annual changes in regulatory requirements. In fact, the rules have become so convoluted that no one, including the staff in charge of implementing them, can fully understand and interpret them.”
The letter discusses three Medicare programs with penalties that impact physicians:
EHR meaningful use
CMS should adopt a more flexible approach for meeting meaningful use, instead of the program’s current all-or-nothing requirements, the letter said. The agency also should make optional measures that are out of physicians’ control, such as those based on interoperability. The letter also asks CMS to reduce burdensome technology requirements that stifle EHR usability and innovation.
Physician Quality Reporting System
Without public, aggregate information on the number of physicians who successfully and unsuccessfully participated in PQRS, there’s no way to assess the program in a timely manner, the letter said.
CMS should release aggregate PQRS data for 2013 so physicians can evaluate the program. The agency should create a more formal appeals process to give physicians more than 30 days to seek correction of any inaccurate information. Finally, CMS should maintain a more robust set of claims-based measures and reporting options to reduce reporting costs.
Value-Based Modifier
The VBM program should be repealed, or at least limited in its implementation, the letter said. If it isn’t repealed, more time is needed to gauge its results on large physician groups before penalties are ratcheted up and extended to small and solo practices.
“The current strategy of plowing ahead with policies that place an ever-increasing burden on both CMS and physicians—combined with the flawed roll-out of the Medicare claims data release and Open Payments program and the problems with these programs—is causing serious damage to the agency’s image and to physician confidence in the government’s stated goal of achieving a health care system that delivers more value for the dollar,” the letter said.
The AMA will continue to advocate for needed changes to these and other regulatory programs.