At Samaritan Health Services, organizational well-being is more than a strategic goal—it’s a deeply rooted value that shapes the culture, care and community.
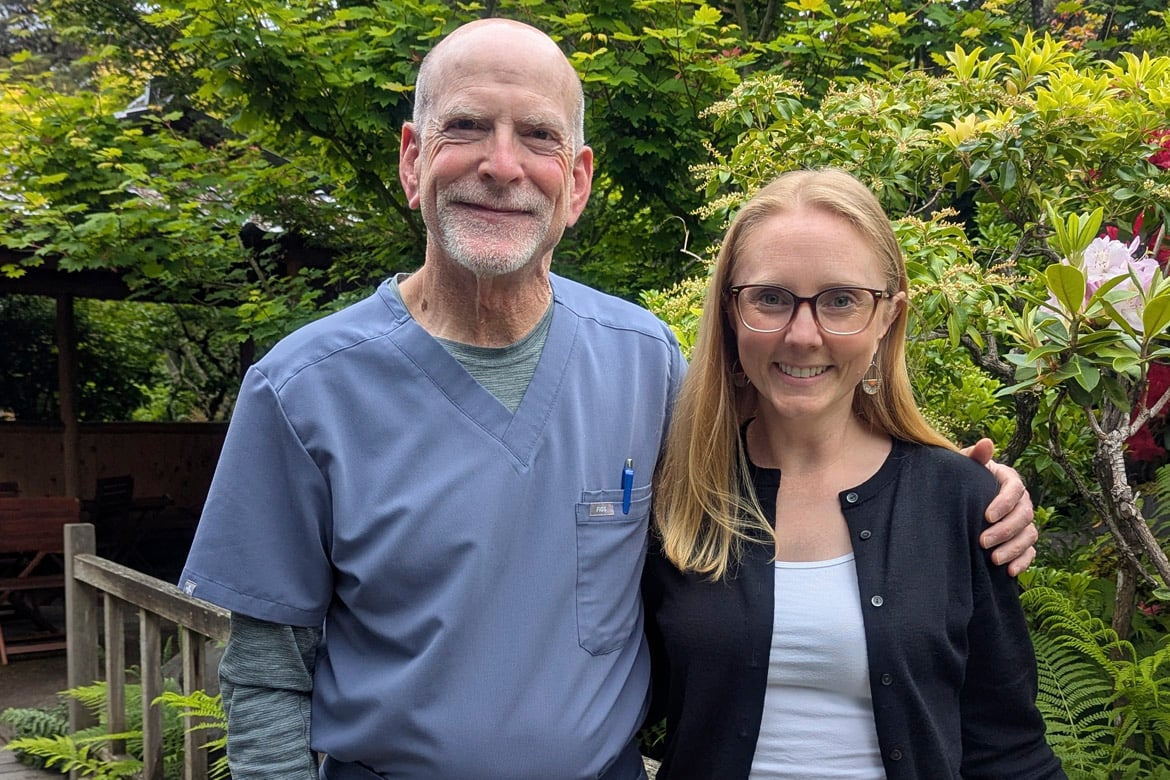
As William Barish, MD, a hospitalist, prepares to retire from his role as chief wellness officer (CWO) at Samaritan Health Services on June 30, he leaves behind a legacy of compassion, innovation and steadfast support for those who dedicate their lives to caring for others.
Stepping into this vital leadership role is Kelsey Terland, MD, a palliative care physician, who brings a fresh perspective and strong commitment to continuing—and evolving—Samaritan’s workforce well-being efforts.
“At its core, organizational well-being is about helping people feel a sense of connection or fulfillment in the work that they do,” said Dr. Terland. To do that, “we have to feel heard and supported by our leadership.”
“It’s about creating an environment where physicians can practice what they spent many years in school and training to do … and connect with their patients, removing as many barriers to that as possible,” said Dr. Barish.
While Dr. Barish is retiring from his CWO role, he will still be practicing medicine and helping Dr. Terland. Their shared vision remains clear: to build a system where physicians feel supported, empowered and valued—because the well-being of those who care for others is essential to the health of everyone.
In this Q&A, Drs. Barish and Terland reflect on the past, present and future of well-being at Samaritan and the evolving role of the CWO.
AMA: How do you see the role of the CWO evolving in the coming years?
Dr. Terland: The work is challenging and there's a lot of work to do. A lot of the foundational work that folks like Dr. Barish have done at Samaritan has laid a good foundation where we recognize the importance of well-being of clinicians. We're talking about well-being when decisions are being made that impact a clinician’s day.
What that evolution looks like—at least what I see for Samaritan—is building on the foundation to create a sense of community in our organization. That deep connection to the work, I worry is feeling a little fragile right now. That's where I imagine having to focus a lot of my energy.
Dr. Barish: I agree with everything Kelsey said. The ongoing role of a chief wellness officer is, hopefully at some point in the future, to make their position no longer necessary.
Everyone in the organization should be asking the question early on in the discussion: What about well-being?
AMA: How do you maintain your own well-being while working to improve it for others?
Dr. Barish: I have a routine. I exercise regularly, I eat reasonably well, I maintain a good positive outlook, and I get good sleep. So, I take care of myself. But honestly, it's one of the reasons why I want to step away. The chief wellness officer is just a bit burned out. I am just getting a little crispy at the edges and I wanted to turn it over to somebody younger with perhaps a brighter flame. I still support the work and I'm still going to be helping out and supporting Kelsey, but having someone step in who perhaps has a slightly different vision and maybe a little more enthusiasm, it's time.
Another thing that I do for my own well-being is that I do have Watson, the therapy dog. Watson is a Bernedoodle, and we’ve trained him with a national organization. We got him in 2022, so just as we were coming out of the pandemic, because I saw that the staff was just fried—especially the nurses. We got Watson, and he comes into the hospital with me a couple times a week as a therapy dog. The staff love him.
We’ve distributed Watson stickers, and everybody has one on their badge or their water bottle. He’s made a difference in other people’s lives and made a difference in my life too.
Dr. Terland: A lot of my well-being and ability to come back to work each day is helped by the things that I do outside of work. I have two younger kids and a partner, and spending time with them is something that's really important to me. As a mom in medicine, balancing those different hats can be really challenging, but it is really important for my own well-being that I don't neglect any of those hats.
I'm a palliative care physician and the work that I do clinically can be really heavy at times. Having strong teams at work, people who I can debrief difficult interactions with or difficult clinical situations with, has been really important. Having people around me who I've built close relationships with at work is also a part of keeping myself well.
AMA: Looking back on your tenure, Dr. Barish, what are you most proud of?
Dr. Barish: I'm most proud of the work we've done with the AMA. We did a project putting registered nurses into clinics about six years ago and that's what first got me involved with the AMA and Dr. Sinsky. Then, of course, applying for—and being recognized by—the AMA Joy in Medicine® Health System Recognition Program. We were awarded silver last fall and that work has really filtered out to a lot of different areas of the organization, some of which the organization has found to be very helpful.
We developed physician leadership training and started an annual physician leader evaluation process based on the AMA suggestions. Our informatics team also developed a well-being dashboard base which allows leadership to see how our clinicians are doing from a community, clinic and individual level.
I kept emphasizing to our leadership that at the end of the day, it's not about getting an award. It's about what works for this organization and what's going to promote well-being amongst our clinical staff. But so far, our needs and the AMA recognition line up well. I would like to be able to apply for gold next year and I’ll continue to help Kelsey with that.
AMA: What advice or guiding philosophy are you passing on to Dr. Terland as she steps into the CWO role?
Dr. Barish: Take care of yourself. Remember to put on your own oxygen mask first. Then communicate. One of the big things that Kelsey is going to do, which is going to be a step up from where I’ve been, is to get out there and listen and connect with people because it’s really important that people feel that they’re being heard. She’s also going to improve our communication of getting information out. She’s going to do a really great job and I would encourage that.
That’s what needs to happen—the communication and listening and getting the information out that clinicians really want to hear and need to hear. Also, continue to integrate with other departments and continue to infuse well-being throughout the organization to eventually make her job no longer necessary.
AMA: Dr. Terland, what inspired you to take on this position and how do you plan to build on Dr. Barish’s legacy?
Dr. Terland: I came to Samaritan almost five years ago and it was actually coming home for me. I grew up in this part of Oregon, but had been away for a long time, so it was nice to come home. I was lucky that my clinical time was out at our critical access hospital in Lebanon where Dr. Barish is one of our hospitalists.
In many ways, I would say that Bill has been one of my primary mentors at Samaritan since I started here in clinical practice, but also in leadership. As I stepped into a medical director position, Bill was really great in helping me figure out how to navigate our system and make sure my voice was being heard by the people who needed to hear it.
Where I came from, we didn’t have a chief wellness officer or a well-being program, at least not that I was aware of. So, the role was novel to me when I met Bill. As I got to know him and the work he was doing, it really resonated with me personally and with who I am as a leader for my own teams. Focusing on taking care of each other and supporting each other so that we can come back to work each day and find meaning in the work that we do has been core to my leadership.
The opportunity to be able to support that on a larger scale within the organization is really exciting to me. That’s what drew me to the idea of stepping into this role.
While I have my ideas about what I think might be helpful, I really need to listen to my colleagues about where they’re hurting and where they need support, then focusing my efforts in the places that will be most impactful.
AMA: What are your top priorities for your first year as CWO and how will you measure success?
Dr. Terland: What I’ve talked a lot with other members of the well-being core team and then other leaders at Samaritan is how we build a culture of well-being. We have these foundational programs that we have connected with and put in place, and now how do we really infuse that into our culture?
One way that we could help with that is looking at how we onboard and orient new clinicians into our system. I joined Samaritan in November of 2020, admittedly a hard time to onboard at an organization, and so certainly my experience is not what I hope for colleagues who are joining the organization today. I know we do it better today than we did in that very hard time, but there's room for us to really start building a culture of well-being with new clinicians from day one.
Bringing new people in and setting up culture is really important, but then we also need to have our folks who are already here and established live and breathe that culture too.
One thing that would help people feel connected to each other and feel like they have purpose and meaning at work and are impacting patients' lives, but also their colleagues' lives would be a mentoring program. That's happening in informal ways in our system and that's meaningful, but I would love to see a more formalized process where we have clinicians supporting and listening to clinicians.
AMA: If you could share one message with physicians about well-being, what would it be?
Dr. Terland: I would say speak up when you have a pebble in your shoe. Make sure that you are letting people know because you can't be the only one struggling with that same pebble. If we can bring awareness to that, then we can do something about it hopefully to help make the day a little bit better.
Dr. Barish: Along the same lines, empowering clinicians to find their voice and speak up to claim the role they have always wanted to have as a physician; as a healer of people.
As the leader in physician well-being, the AMA is reducing physician burnout by removing administrative burdens and providing real-world solutions to help doctors rediscover the Joy in Medicine.
AMA STEPS Forward® open-access toolkits and playbooks offer innovative strategies that allow physicians and their staff to thrive in the new health care environment. These resources can help you prevent burnout, create the organizational foundation for joy in medicine, improve practice efficiency and cultivate leadership.