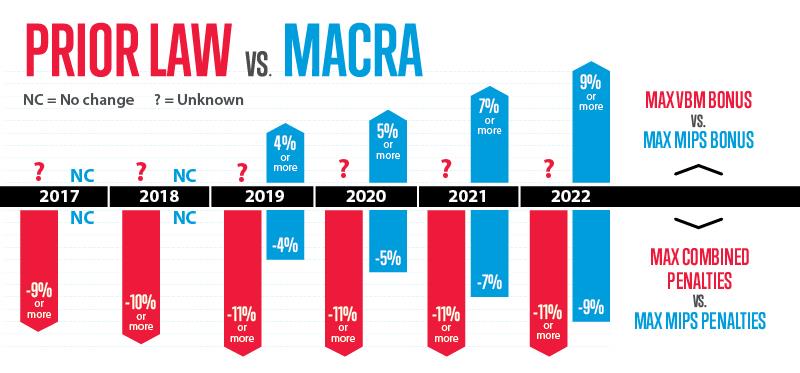
Regulatory penalties under the current Medicare payment system have been rising, overwhelming physicians with reporting burdens just to avoid payment cuts. But how will financial penalties and bonuses change in the new system? Under the Medicare Access and CHIP Reauthorization Act (MACRA), regulatory penalties starting in 2019 will be much less severe, and physicians will have greater opportunity for bonuses.
How MIPS will be different
The current pay-for-performance programs—the Physician Quality Reporting System (PQRS), the value-based payment modifier (VBM) and the Meaningful Use electronic health record program—each judge physicians separately on various metrics.
Under MACRA, physicians who remain in Medicare’s fee-for-service program will participate in the Merit-based Incentive Payment System (MIPS). Though improvements to the proposed regulatory framework are needed for implementing MIPS, there is no question that the system offers improvements over current Medicare law.
MIPS consolidates and better aligns the separate quality and performance measurement programs that currently affect physicians’ payments. It adds one new component—clinical practice improvement activities—with a menu of more than 90 activities through which physicians can demonstrate high-value services and receive credit.
The current system includes quality measures that overlap and sometimes conflict. For instance, a physician who did not successfully report under PQRS automatically received a second negative payment adjustment under the VBM. With MIPS, that will no longer be the case. In addition, CMS is proposing to reduce the number of quality measures that physicians must report, as well as allowing greater flexibility in their choice measures.
Also in the current system, the Meaningful Use and PQRS programs were scored on a pass/fail approach, which required physicians to be 100 percent successful on all reporting requirements to avoid penalties.
Under the MIPS, physicians will receive partial credit for elements they are able to report on successfully, have the chance to earn bonuses if they score above average performance thresholds and avoid penalties if they meet those thresholds.
As the table illustrates, financial risk regarding penalties will be significantly less under MIPS than it was under the previous system. The future severity of VBM penalties and bonuses under prior law is unknown because CMS ceased proposing them after MACRA passed; prior to MACRA’s passage, the penalties and potential bonuses increased each year.
MIPS is characterized by not only a change in penalties but also a new bonus structure that increases as the program moves forward each year. Learn more about MACRA in the AMA’s MACRA Action Kit.