Although measuring blood pressure may seem like a normal routine in most physicians’ office workflows, seven seemingly minor factors can artificially inflate patients’ blood pressure measurements.
For Kim Hardy, MD, a family medicine physician with Prohealth Care  Medical Associates in Sussex, Wisconsin, a simple reminder helped her avoid needlessly adjusting medications for a patient. Dr. Hardy and her staff use a blood pressure management chart she learned about via the AMA’s Twitter feed as a daily cue to ensure patients’ blood pressure measurements are as accurate as possible.
Medical Associates in Sussex, Wisconsin, a simple reminder helped her avoid needlessly adjusting medications for a patient. Dr. Hardy and her staff use a blood pressure management chart she learned about via the AMA’s Twitter feed as a daily cue to ensure patients’ blood pressure measurements are as accurate as possible.
“I recently had a patient in the office whose blood pressure remained significantly elevated after repeated measurement,” Dr. Hardy said. “I asked her if she needed to use the restroom, and she said she did. After emptying her bladder, her blood pressure reading was to the goal of less than 140/90. My medical assistants were amazed.”
“It prevented me from having to readjust [the patient’s] medications,” she said.
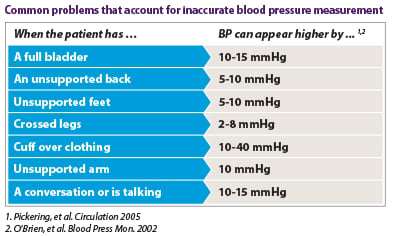
Falsely high blood pressure measurements can lead to unnecessary prescriptions and potentially harmful medication doses. Monitor these seven factors to prevent an inaccurate blood pressure reading:
- The patient has a full bladder.
- The patient’s back is unsupported.
- The patient’s feet are unsupported.
- The patient’s legs are crossed.
- The sphygmomanometer cuff is over clothing.
- The patient’s arm is unsupported.
- The patient is talking or hasn’t had at least three minutes of quiet time prior to the measurement.
Incorporating evidence-based principles like these into practice workflows is a key element of the AMA’s Improving Health Outcomes initiative. A pilot program involving multiple clinical sites in two states is implementing principles of safe design into the ambulatory setting to improve outcomes around hypertension. Similar approaches, such as hospitals using checklists to reduce central-line infections, have seen successful results.
To apply safe design principles to blood pressure management, the AMA is collaborating with pilot sites and researchers at Johns Hopkins Medicine Armstrong Institute for Patient Safety and Quality and the Johns Hopkins Center to Eliminate Cardiovascular Health Disparities to develop and test a set of evidence-based recommendations, based on a simple framework called the “M.A.P. for achieving optimal hypertension control”:
- Measuring blood pressure accurately every time it’s measured
- Acting rapidly to address high blood pressure readings
- Partnering with patients to promote self-management of high blood pressure
The pilot sites are integrating best evidence into each step of the M.A.P. framework. For example, the AMA is incorporating successful elements of a program at Johns Hopkins Center to Eliminate Cardiovascular Health Disparities in designing resources to help practices engage patients in better self-management.
Stay connected for additional insights: Follow the AMA on Twitter to get timely tips as Dr. Hardy did about this issue and other topics of importance to your practice.