At the start of summer, New Orleans took initial steps to reopen—the mask mandate had been lifted, restaurants were opening, hotels were full, and the city seemed alive again. As a city that celebrates, there was optimism that everyone would be together again to celebrate a delayed Jazz Fest in October. But COVID-19 had other plans. The Delta variant snuck up and wave four of the pandemic came crashing down and it seemed like the city was back where it started, this time with the added complication of Hurricane Ida.
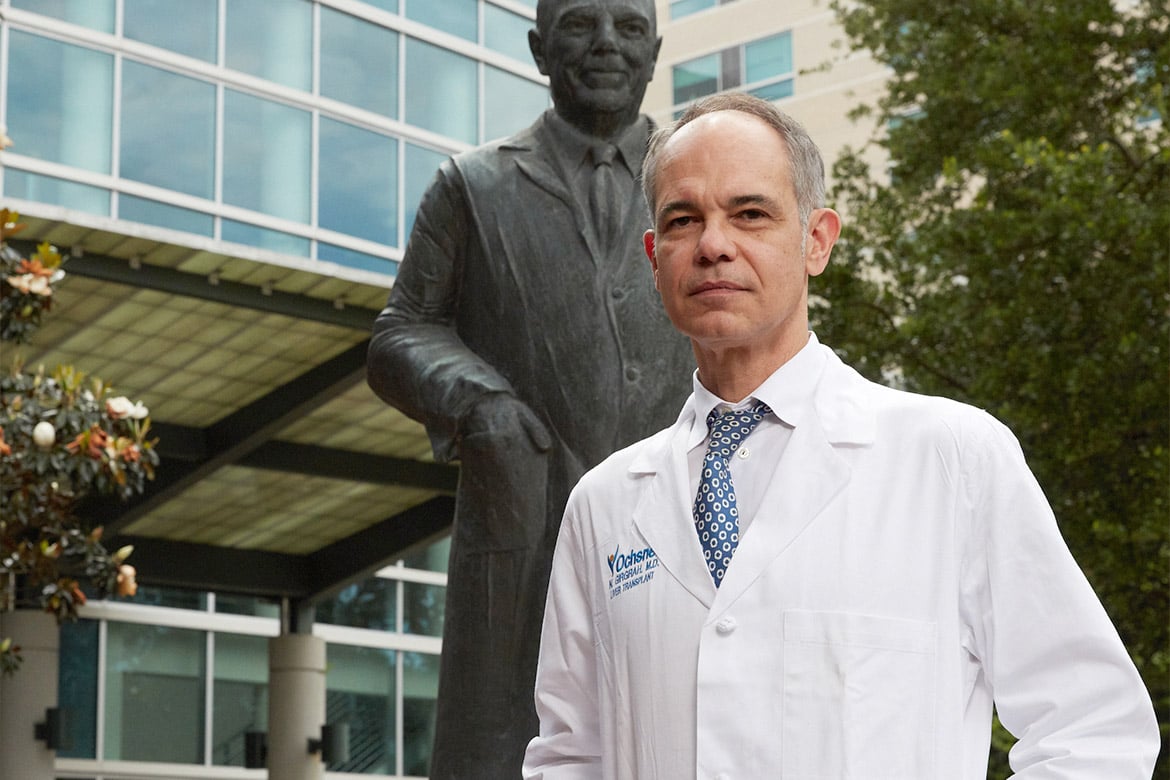
As the fourth wave of the pandemic hit New Orleans, AMA member Nigel Girgrah, MD, PhD, saw a lot of anger that he hadn’t seen previously, even in himself. Dr. Girgrah is a transplant hepatologist and chief wellness officer at Ochsner Health—an AMA Health System Program member. He is also the medical director of the Liver Transplant Program at Ochsner.
During a recent interview, Dr. Girgrah discussed the impact of low vaccination rates, Hurricane Ida and physician burnout, and how Ochsner continues to focus on the well-being of its workforce.
AMA: How were you feeling through all of this?
Dr. Girgrah: I was finally feeling that my kids’ lives were resuming some normalcy—that there wouldn’t be masks in school. So, I was upset when things got worse. I stay out of the fray on social media, but for the first time in my life I was engaging in this heated social media exchange on Facebook with one of my friends. I realized that it wasn’t making me feel any better, and it certainly didn’t change his opinion. It caused me to pause and to try and just focus on our community purpose—our patient mission.
I sent out an open letter in August about feeling betrayed. I tried to put into words my own feelings. This open letter went out to all our employees—over 30,000—to try and really remind people about how important Ochsner is to our community, to our patients, and that this was a virus that didn’t discriminate.
What we were seeing, not surprisingly, was just complete exhaustion. And this was before Hurricane Ida. When I reflect on the first surge back in March and April of 2020—we were a big, big hot spot up there with New York and Los Angeles. But at that time, there was a sense of health care professionals being heroes. ... But now that was wearing a little thin. It wasn’t happening anymore.
The other thing was the incredible workforce shortage with nurses. Unlike previous surges, we couldn’t really attract the agency nursing because the whole country was being affected by the pandemic. So that was something that was really stretching folks and leading to exhaustion, burnout and certainly, for some, post-traumatic stress disorder [PTSD].
The week of Aug. 9, we peaked in terms of hospitalizations due to COVID-19. It was close to 1,100 within our health system and that was unbelievable. The fourth surge was the largest number of patients we had hospitalized. That started to decline a little bit in August, but even the week that Ida came in, we were between 700 and 800 hospitalizations. We were nowhere near being over this incredible fourth wave.
AMA: Was there more exhaustion, PTSD, frustration and anger at this point?
Dr. Girgrah: Yes. The interesting thing is, we did the first AMA organizational biopsy—an expanded burnout assessment survey—to further understand key system level drivers that take away from organizational and professional well-being. That went out just at the beginning of the fourth surge. So, we actually—at least among our physicians and advanced practice providers [APPs]—had an opportunity with the survey to inquire about things like PTSD, and to look at areas around post-traumatic growth as well and how we can shift the mindset and the conversation. This was before the fourth surge, but we were looking at about 21% of our employed physicians and APPs meeting the criteria for PTSD.
AMA: What else did you find from that survey?
Dr. Girgrah: We, as an organization, were one of the 44 organizations to receive the AMA Joy in Medicine™ Recognition Program award—and one of five organizations to receive gold recognition. That’s basically something that rigorously looks at commitment to well-being.
While we’ve put a lot in place, pre-pandemic we had seen our burnout rates go down significantly. With the survey, we did see—not surprisingly—that those gains made at reducing burnout, there was a bit of a setback, certainly with the 18 months of the pandemic.
We’re seeing higher rates of burnout. Certainly, our folks telling us that there was values alignment within our organization, that wasn’t the issue. It was just a lot of fatigue, descriptions of workforce shortages and things like that.
AMA: What happened once Hurricane Ida hit New Orleans?
Dr. Girgrah: Most times with hurricanes, it seems like they're on our radar screen. For seven days, we're following these things. But this one really snuck up on us. It hit us on the 16th anniversary of Hurricane Katrina, which was kind of spooky.
Ida seemed to creep out of nowhere. Luckily, we’re a resilient organization. Preparing for emergencies is in our wheelhouse—that’s a result of having gone through many weather-related disasters. We're an organization that was prepared, but it was an additional big sucker punch on top of everything else.
I'm not surprised, but incredibly proud of how our organization stepped up. It gets down to working down Maslow's hierarchy of needs again and being able to provide for our employees and for our community— the basic needs. You can't focus on yourself, your families or your community if you don't have shelter, if you don't have water, if you don't have gas to get back and forth to work.
We managed to import gasoline. I saw pictures of our executives actually pumping gasoline for our workforce to enable them to come back and forth to work. And for those employees who have been devastated [by the loss of housing], we put up shelter by collaborating with hotels to provide rooms for employees so that they could continue to work and protect their families as well. It was an incredible response, but it’s been like nothing I’ve seen.
It wasn’t horribly bad for New Orleans, but for my colleagues in the Bayou—which is about an hour from here—that community was completely devastated. We had to evacuate our patients from two of our community hospitals—inpatients at Chabert Medical Center in Houma and Ochsner St. Anne Hospital in Raceland, Louisiana—to other hospitals. Luckily, we’re a health system, so we’re able to do that. We’re able to capitalize on our willingness to be a true health care system and to focus on teamwork.
AMA: Is following Maslow's hierarchy of needs how you help physicians and other health professionals cope with this added stress?
Dr. Girgrah: Pre-pandemic as an organization, and as an office of professional well-being, we were focused on many items at the top of Maslow's hierarchy of needs. But the pandemic really necessitated moving down the hierarchy of needs.
Early on in the pandemic, people couldn’t come to work if they were worried about their own health and safety, if there was going to be enough PPE [personal protective equipment], if there was going to be child care. These are things our organization has focused on and really done an excellent job of communicating what we’re doing. That continues through the various incarnations of COVID-19 and certainly through the hurricane.
I am hearing from our physicians and APPs—and we saw this in the survey—that while that’s been received very well, certainly there’s been a thirst for resilience offerings. There’s also been a desire to have more authentic conversation about mental health. There’s been a need to diversify our mental health offerings, but what’s coming across loud and clear is that we also need to get back to walking and talking with professional fulfillment. That’s getting back to practice efficiency and leadership development.
As we emerge from the pandemic, there’s going to be a need for renewed focus on doubling down on our efforts to improve efficiency of work in our environment.
AMA: How do you continue to push forward and keep physician well-being front and center?
Dr. Girgrah: We're starting up the work groups that we had in place pre-pandemic—very engaged, multidisciplinary work groups around practice automation and innovation. So, work groups around our EHR, advanced team-based care and provider communication—those are being rebooted.
There have been some silver linings with the pandemic. While we all acknowledge that Zoom isn't necessarily an ideal way to connect, it has allowed us to bring people together in a bit more of a nimble fashion and very quickly understand what’s going on throughout our health system. Those efforts are being rebooted and rebooted in a big way.
We’re also an organization that’s committed to measuring these things, measuring not just the primary measures of success like engagement, burnout, PTSD, post-traumatic growth, but looking at secondary measures of success, measuring how hard our folks are working outside normal work hours and teamwork. You can’t improve things unless you’ve established measurements of success that you’re willing to tackle. We’re certainly committed to those things.
AMA: What kind of lasting impact do you think the pandemic will have for the doctors and health professionals at Ochsner?
Dr. Girgrah: It would be ridiculous to think that as we emerge from the pandemic—or as we plug through the pandemic—that there isn't going to be a toll that we're going to see in our community and our workforce. It's allowed us to think differently. ... It’s about being a little more vulnerable and authentic when you're talking to your team.
Talking about struggles that I may be having and communicating those—that leads to trust. We are seeing many leaders lead with vulnerability, but it's also allowed our organization to be a little more innovative in thinking about how to meet the mental health needs.
We’ve always been an innovative health care system, and how we respond to the pandemic and mental health needs of our workforce is an example of that. The pandemic and the hurricane have demonstrated, once again as Katrina did, what an incredibly resilient organization we are and that's built upon the resilience of our teams, our employees and our workforce. I couldn't be prouder.