The number of health care business transactions conducted electronically continues to grow, saving physician practices time and money. But two types of transactions continue to lag way behind: Prior authorization and attachments used in the submission of additional information—frequently to support a prior authorization request or appeal.
The most recent report published by the Council for Affordable Quality Healthcare (CAQH) tracking the health care industry’s annual progress toward automating basic transactions shows these types of transactions bringing up the rear. While 97% of claims are sent electronically, as are 90% of eligibility and benefit verifications, only 28% of prior authorizations are processed electronically. Similarly, only 24% of attachments are submitted electronically, and human interactions involving phone calls, faxes, email or standard mail are still heavily relied on in their transmission.
The CAQH Committee on Operating Rules for Information Exchange (CORE) is a multistakeholder collaboration of health plans, health care professional groups—including the AMA—and other industry organizations that develops national operating rules for electronic business transactions. These rules bring consistency to electronic communication between physician practices and health plans that improve the value and utility of transactions—and spur adoption.
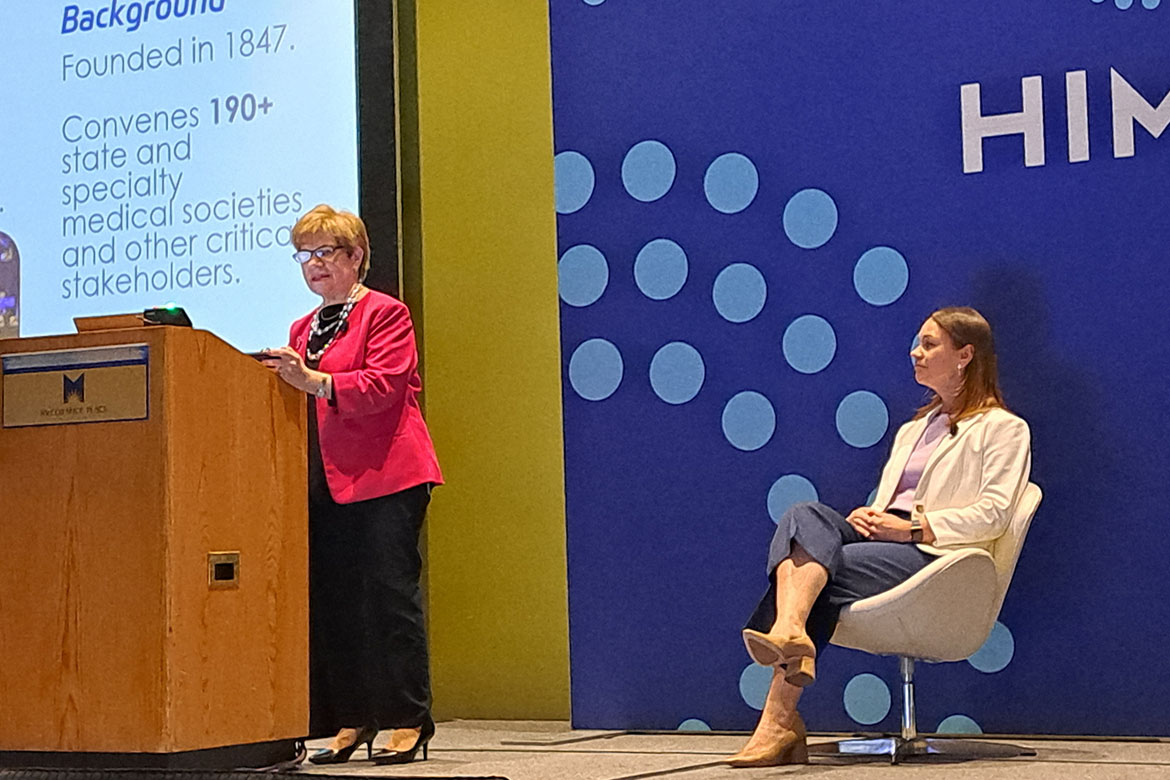
“I like to think of operating rules as the secret weapon behind interoperability and revenue cycle,” CAQH Core Vice President Erin Weber said during a presentation at the Healthcare Information and Management Systems Society’s (HIMSS) Global Health Conference, held in Chicago.
Weber was joined by AMA Trustee Marilyn Heine, MD, who noted that the AMA is advocating that CAQH CORE’s updated operating rules should be mandated by the National Committee on Vital and Health Statistics (NCVHS), as they will ease prior authorization and other administrative hassles.
Reducing physician burnout and fixing prior authorization are critical components of the AMA Recovery Plan for America’s Physicians.
Far too many physicians experience burnout. That's why the AMA develops resources that prioritize well-being and highlight workflow changes so physicians can focus on what matters—patient care.
Prior authorization is overused, and existing processes present significant administrative and clinical concerns. Find out how the AMA is tackling prior authorization with research, practice resources and reform resources.
Streamlining the business of health care
AMA support took the form of both oral testimony and a letter in response to a NCVHS request for comment regarding updated transaction standards and operating rules.
“The AMA strongly believes that federal adoption of the updated operating rules will benefit physicians and their staff through improved workflow efficiencies, reduced time spent on administrative tasks, increased time for patient care, and addressing unmet and emerging business needs,” AMA CEO and Executive Vice President James L. Madara, MD, wrote in a letter to the NCVHS (PDF). “We further expect that the rules will positively impact patients.”
Dr. Heine called the new operating rules for prior-authorization attachments “a long-awaited step to streamline the prior-authorization process.” She highlighted multiple benefits offered by the rules, including support for document reassociation by plans; minimum file size specification, which avoids costly resubmissions; and requirements for maximum-response times, acknowledgments and handling of errors.
Dr. Heine also walked through several patient case studies to illustrate the real-world value of other rules in the CAQH CORE package:
- The updated eligibility-and-benefits rule requires plans to include information regarding telehealth coverage and prior authorization needs.
- Updated infrastructure rules increase system availability from 86% to 90%, reducing delays due to system downtime.
- Revised connectivity requirements protect the security, accuracy and integrity of patient health information.
- A new rule requires health plans to include patient attribution information in eligibility responses, supporting physician success in value-based payment models.
Reducing burden and burnout
“Once implemented, effective rules can help physicians maximize our focus on patient care,” said Dr. Heine, a member of the CAQH CORE board and a clinical assistant professor of medicine at the Drexel University College of Medicine.
“The net result is the reduced administrative burden and physician burnout,” Dr. Heine said.
The hassles of doing business with many different health plans—all with their own individual business requirements—introduces time-consuming complexity into revenue cycle processes for physician practices. Operating rules rein in these problems by bringing much-needed uniformity to electronic transactions.
“AMA studies have shown that there are high levels of physician administrative burden and burnout and that these are linked. These may be mitigated by operating rules that streamline prior authorization and related business practices as well as ensure interoperability from all of the health plans with which a practice does business,” Dr. Heine said.
The AMA and the American Hospital Association sent a follow-up letter (PDF) to NCVHS urging the committee to recommend federal adoption of the CAQH CORE operating rules because they address “critical unmet business needs in health care, as well as emerging industry trends.”