If you’re preparing for the United States Medical Licensing Examination® (USMLE®) Step 1 exam, you might want to know which questions are most often missed by test-prep takers. Check out this example from Kaplan Medical, and read an expert explanation of the answer. Also check out all posts in this series.
This month’s stumper
A 16-year-old girl is brought to the emergency department because of acute abdominal pain and diarrhea. She has had three similar episodes, but no cause has been found. She also complains of burning on urination. The patient appears diaphoretic and in pain. Her temperature is 102 °F (38.8 °C) and pulse is 95 beats per minute. Physical examination shows there is diffuse abdominal tenderness, especially around the suprapubic area. First percussion over the costovertebral angle elicits exquisite pain on the right.
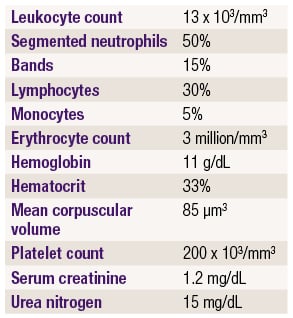
Laboratory studies show:
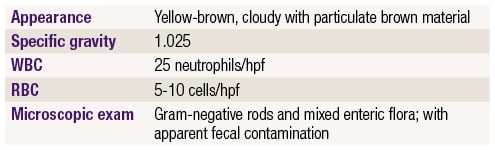
Urinalysis shows:
Which of the following is the most likely condition?
A. Celiac disease.
B. Crohn disease.
C. Diverticulitis.
D. Renal colic.
E. Renal stone.
F. Ulcerative colitis.
G. Whipple disease.
The correct answer is B.
Kaplan Medical explains why
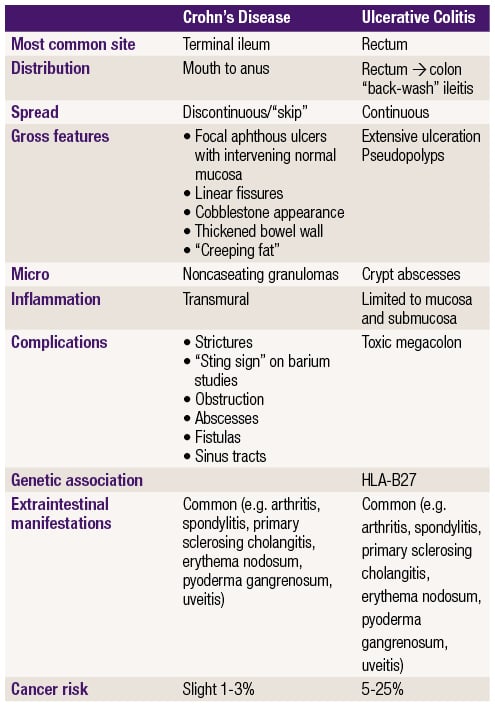
This patient most likely has an enteric fistula to the bladder (enterovesicular fistula) as evidenced by mixed bacterial flora and Gram-negative rods in the urine along with brown fecal contamination. Fistulas are seen with Crohn disease, in which patients can present with repeated bouts of diarrhea and abdominal pain, sometimes with additional symptoms (see table below). Other fistulas that occur with Crohn disease include enterocutaneous fistula (common in the perineum or abdominal areas) and enteric fistulas between bowel segments (causes obstruction).
Fistulas occur in patients with Crohn disease because the inflammatory process involves the entire bowel wall (transmural inflammation). In ulcerative colitis (choice F), inflammation is generally relegated to the mucosa and submucosa.
This patient's fistula into the bladder has likely caused pyelonephritis, as evidenced by costovertebral angle tenderness on the right. One would expect elevated temperature and slightly elevated heart rate, as seen here. Additionally, the patient's lab values should show an increase in WBC count with left shift.
The other differences between Crohn disease and ulcerative colitis are shown in the table, with one caveat: primary sclerosing cholangitis (PSC) is associated with both diseases, but it is more common in UC than Crohn disease.
Why the other answers are wrong
Choice A: The distinctive feature of celiac disease is malabsorption due to gluten sensitivity. The malabsorption generally improves with removal of gluten from the diet. Celiac disease can present with diarrhea and abdominal discomfort from bloating, and can involve the proximal small intestines, but there is no association with fistula formation.
Choice C: Diverticulitis can present with abdominal pain and fever but is usually a disease of older adults. Divericular outpouches can become inflamed and rupture, leading to peritonitis, but fistulas rarely occur.
Choices D and E: Renal colic due to a stone would cause pain referred to the back and would not be expected to cause a polymicrobial bladder infection.
Choice F: Fistulas occur in patients with Crohn disease because the inflammatory process involves the entire bowel wall (transmural inflammation). In ulcerative colitis , inflammation is generally relegated to the mucosa and submucosa.
Choice G: Whipple disease is a small intestinal malabsorption syndrome that has been related to microbial infection (macrophages can be seen containing bacilliform bodies that have been identified as Tropheryma whippelii). Whipple disease is more commonly seen in older males and presents with fever, general malaise, fatigue, lymphadenopathy, and weight loss. It will not, however, cause fistula formation into the bladder resulting in polymicrobial bladder infection.
Tips to remember
- Gastrointestinal diseases are notorious for producing symptoms that may be difficult for a doctor to evaluate accurately.
- Suspect a enterovesicular fistula secondary to Crohn disease in a patient with longstanding abdominal pain who develops brownish-yellow urine (due to fecal contamination) with multiple enteric organisms.
For more prep questions on USMLE Steps 1, 2 and 3, view other posts in this series.