If you’re preparing for the United States Medical Licensing Examination® (USMLE®) Step 1 exam, you might want to know which questions are most often missed by test-prep takers. Check out this example from Kaplan Medical, and read an expert explanation of the answer. Also check out all posts in this series.
This month’s stumper
A 38-year-old woman comes to the physician because of excessive thirst and urination for the past four weeks. Her appetite is increased, but she has lost 6.8 kg (15 lbs.) in one month. Her temperature is 37.5°C (99.5°F), pulse is 87 per minute, respirations are 15 per minute, and blood pressure is 142/88 mm Hg. Physical examination shows erythematous necrotizing skin eruptions on her legs. Her fasting blood glucose is 170 mg/dL and a gastric acid test reveals normal gastric acid volume and a pH of 2.0. A CT scan shows a tumor in the tail of the pancreas.
Which of the following is the most likely cell from which the pancreatic tumor is derived?
A. Acinar cell.
B. Alpha cell.
C. Beta cell.
D. Delta cell.
E. G cell.
The correct answer is B.
Kaplan Medical explains why
The symptoms described are typical for a patient with glucagon excess secondary to a glucagonoma. Increased glucagon causes a syndrome similar to diabetes mellitus with increased thirst/appetite, weight loss, and excessive urination (glucose acts as an osmotic agent in the kidney). Glucagon increases glycogenolysis and gluconeogenesis in the liver, resulting in elevated systemic glucose levels. However, in these patients, insulin-producing beta cells are still functional; thus, extremely elevated glucose levels and diabetic ketoacidosis are rare.
Glucagon is secreted by alpha cells of the pancreatic islets of Langerhans. Increased levels are rare and are usually due to carcinoma (70%) or adenoma (30%) of the islets. Patients also have migratory skin rashes (necrolytic migratory erythema), alopecia, hyperpigmentation of the skin and glossitis. Diagnosis is made by measuring glucagon levels. Treatment includes surgical resection and octreotride (somatostatin) to reduce glucagon output.
Why the other answers are wrong
Choice A: The acinar cell, the main exocrine cell of the pancreas, contains digestive enzymes. Auto-digestion of the pancreas by premature activation of these enzymes (especially amylase and lipase) occurs in pancreatitis. Acute pancreatitis is an emergent medical condition characterized by abdominal pain radiating to the back (retroperitoneal organ) and elevation in serum amylase/lipase. Chronic pancreatitis produces chronic abdominal pain and is associated with fibrosis and atrophy of the acinar structures, and pseudocyst formation.
Choice C: Beta cells are responsible for insulin release. An adenoma of beta cells (insulinoma) would cause hyperinsulinism. Insulin ultimately decreases serum glucose through inhibition of glucagon and increased uptake of glucose by muscle and adipose tissue (via GLUT-4 receptor), thus decreasing glucose availability for other organs. Symptoms of hypoglycemia include dizziness, confusion, sweating, anxiety, and tachycardia. These symptoms result from a combination of adrenergic activation (epinephrine can mobilize glucose stores) and decreased glucose availability for the brain. Glucose needs to be given promptly to avoid coma and death. The characteristic lab findings with insulinoma is elevated insulin and C-peptide plus decreased blood glucose. The C-peptide helps distinguish an insulinoma from exogenous/surreptitious insulin use (C-peptide is only produced in pancreas and is not found in injected synthetic insulin).
Choice D: Delta cells are islet cells that secrete somatostatin. Somatostatinomas are usually malignant. Clinically, a diabetes mellitus-like syndrome occurs (via somatostatin inhibition of insulin) along with diarrhea/steatorrhea (via somatostatin inhibition of pancreatic lipase/bicarbonate release) and cholelithiasis (via somatostatin inhibition of CCK and gallbladder contractility). Diagnosis is made from elevated serum somatostatin levels, but can be difficult because of the hormone's short half-life.
Choice E: The G cell is the islet cell that secretes gastrin. Gastrin excess is usually associated with gastrinomas, 70% of which are malignant. Zollinger-Ellison syndrome causes low gastric and duodenal pH, multiple gastric/duodenal ulcers, and diarrhea/steatorrhea (low pH inactivates pancreatic enzymes). Diagnosis is made from high serum gastrin levels and a secretin stimulation test.
Many of these pancreatic islet cell tumors can be found as part of multiple endocrine neoplasia type I (MEN I), a neuroendocrine syndrome characterized by a triad of pituitary adenoma + hyperparathyroidism + pancreatic islet cell tumors.
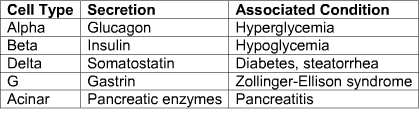
Consult the following table for additional review:
Tips to remember
Glucagon excess:
- Rare, but usually due to carcinoma (70%) or adenoma (30%) of alpha cells of the islets of Langerhans.
- Syndrome similar to diabetes mellitus with hyperglycemia.
- Other findings include migratory skin rashes, alopecia, hyperpigmentation of the skin, and glossitis.
For more prep questions on USMLE Steps 1, 2 and 3, view other posts in this series.
The AMA and Kaplan have teamed up to support you in reaching your goal of passing the USMLE® or COMLEX-USA®. If you're looking for additional resources, Kaplan provides free access to tools for pre-clinical studies, including Kaplan’s Lecture Notes series, Integrated Vignettes, Shelf Prep and more.