A final rule published last week by the Centers for Medicare & Medicaid Services (CMS) implements a proposal giving more options to physicians trying to meet electronic health record (EHR) meaningful use requirements this year.
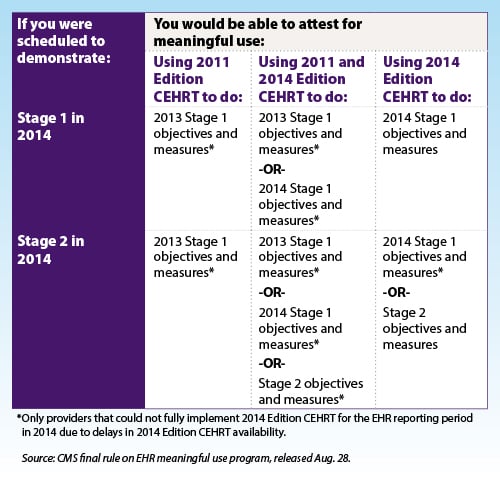
The rule allows physicians to use older certified EHR technology (Version 2011), a combination of old and new technology (Versions 2011 and 2014) or just new technology (Version 2014) in order to meet meaningful use requirements this year. And physicians who were scheduled to move to Stage 2 this year instead will be allowed to meet Stage 1 requirements for an additional year.
While the changes are helpful to some degree, they do not address the overarching problem with the meaningful use program: The 100 percent pass/fail policy places physicians at risk for financial penalties, even if all they fail to meet is a single measure.
Key provisions of the final rule physicians
- The changes only apply to physicians whose certified EHR technology (CEHRT) was not “fully functional” this year and who experienced “delays” in receiving their upgraded software. Physicians who encountered delays that impacted their ability to train staff, test upgrades or establish new work flows would qualify to take advantage of the changes.
- The changes do not apply to physicians who experienced the following challenges associated with implementing 2014 software:
- Financial issues or costs to upgrade, install, test and so forth
- Challenges meeting the meaningful use objectives or measures (with some very limited exceptions)
- Staff changes or turnover
- Physician “inaction,” which led to delays in upgrading software
- For physicians who practice at multiple locations, denominators should be limited to patient encounters at locations that are equipped with Version 2014 software that has been fully implemented for more than 50 percent of the patient encounters during the reporting period.
- Medicaid physicians in their first year of meaningful use are required to purchase Version 2014 software.
- The changes finalized in this rule are applicable to 2014 reporting periods only.
The AMA is reviewing the impact of this rule on quality requirements and will provide more details shortly. View a table from the Aug. 28 final rule to see the options physicians have for meeting measures using different software versions.
CMS also clarified that physicians who are just starting meaningful use this year and who are unable to meet the Oct. 1 attestation deadline still can attest for the last 90 days of the year and qualify for an incentive for 2014 data. That attestation deadline is Feb. 28. In addition, CMS made several other changes to Stage 1 in an earlier rule published in 2012. A complete list of these changes is available in a chart developed by the AMA.