When patients present with issues, physicians look to the most effective tools for treatment. The same is true in addressing an epidemic. While much more work remains to reverse the nation’s opioid epidemic, using tools such as prescription drug monitoring programs (PDMP), medication-assisted treatment and naloxone, physicians are making progress. A new fact sheet provides some evidence of that progress on a number of fronts.
Focused prescribing practices
In a fact sheet released by the AMA, physicians’ progress to reverse the nation’s opioid epidemic was quantified showing new trends in the use of available tools. The data was collected from AMA surveys, IMS Health, the Drug Enforcement Administration Office of Diversion Control (DEA), the Substance Abuse and Mental Health Services Association (SAMHSA), the Centers for Disease Control and Prevention (CDC), and the American Journal of Public Health.
In October 2015, the AMA and many medical and other health care organizations joined the President in Charleston, W.Va., to commit to clear metrics to reduce the nation’s opioid epidemic. Though there is still more to be done, the numbers show some progress.
Every state in the nation saw a reduction in opioid prescribing in 2015, which amounted to a 10.6 percent decrease nationally, IMS Health reported. Though these decreases are important, physicians need to ensure that patients with pain receive comprehensive—and compassionate—treatment. While the nation’s opioid supply will almost certainly continue to decrease, providing patients with a full range of evidence-based, non-opioid and non-pharmacologic treatments becomes crucial.
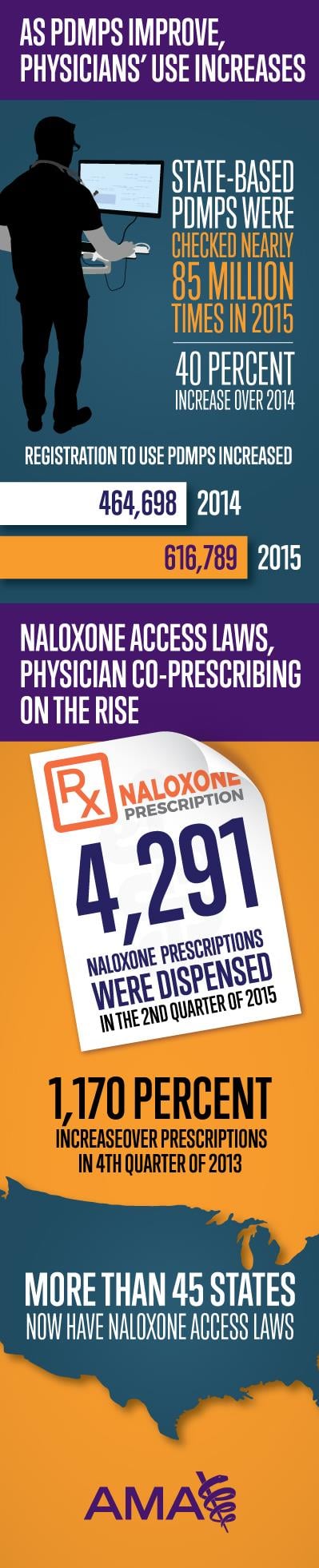
PDMP use can play a significant role in combating the epidemic. These tools contain information on whether a patient is receiving multiple prescriptions from multiple pharmacies and can be helpful in clinical decision-making. State-based PDMPs were checked nearly 85 million times in 2015, a 40 percent increase over 2014, an AMA survey found.
Several states recently implemented PDMPs, including Pennsylvania in August. Registering for these tools is critical to reversing the opioid epidemic and has been a recommendation of the AMA’s Task Force to Reduce Prescription Opioid Abuse since its conception in 2014.
Registration for PDMPs increased by over 150,000 physicians and other health care professionals nationally from 2014 to 2015 and these increases were seen in states with and without mandated PDMP use.
“Physicians and other health care professionals have increased their use of the state’s [PDMP] every year,” said Patrice A. Harris, MD, chair of the AMA Board of Trustees and the AMA Task Force to Reduce Prescription Opioid Abuse in The Olympian. “We need to address opioid addiction and overdose across the entire spectrum, from prevention to treatment.
Education and medication assisted treatment increases
Between 2012 and 2016, the nation saw an 81 percent increase in physicians certified to treat substance use disorders, data from the Substance Abuse and Mental Health Services Association (SAMHSA) showed. That’s more than 33,000 physicians across all 50 states.
Medication-assisted treatment, such as buprenorphine, can help patients with opioid use disorders recover safely and stick to their recovery plans. Prescriptions to help treat opioid use disorder increased by 11 percent from 2014 to 2015. These medications are becoming more common as substance use disorders are recognized as a chronic disease and not a moral failing.
The AMA survey also showed that nearly 50,000 physicians had participated in educational activities related to opioid prescribing, pain management or other related areas since October 2015. The AMA will soon release continuing medical education tools including a primer on the opioid epidemic and two state-specific physician toolkits in Rhode Island and Alabama in cooperation with the state medical associations and governors’ offices. The toolkits will highlight key resources to help reduce opioid-related harm, provide guidance on prescribing practices and direct patients to additional resources in these states.
Naloxone helps reduce overdose
Fifteen states saw reductions in the number of overdose deaths in 2014 compared to 2013. These reductions occurred in the midst of increased co-prescribing of naloxone, the life-saving opioid overdose reversal antidote. The second quarter of 2015 saw a massive 1,170 percent increase in naloxone prescriptions over the fourth quarter of 2013.
“Naloxone can and will save lives, and while co-prescribing the drug is important, it’s simply not enough,” Dr. Harris said in an op-ed for TribTalk. “Naloxone must be accessible and affordable. For this to happen, insurers must cover the medication and offer it to individuals at a reasonable price.”
The physician role in the epidemic is an important one—and the physicians of the nation are recognizing that role and taking it on with vigor, as the numbers show. There is still much to be done, but the effort and motivation is there.
The AMA and other organizations have long been pressing for state legislation to increase access to naloxone and, as of today, more than 45 states have naloxone access laws.