Remember the dramatic results that came from hospitals using checklists to reduce central-line infections? Physicians involved in a new pilot program do, and they’re hard at work to determine how the safety principles behind those checklists can be applied to improving outcomes for one of the most common and dangerous conditions in America: hypertension.
Participants in the pilot program, part of the AMA’s Improving Health Outcomes initiative, are working alongside the creator of the checklist approach, Peter Pronovost, MD, of the Johns Hopkins Armstrong Institute for Patient Safety and Quality, to apply proven patient safety principles from the acute care setting to care in the ambulatory setting.
Just as the checklist safety principles are intended to avoid patient harm, ensuring quality care in screening for and treating patients with high blood pressure can prevent the development of heart disease and stroke down the road.
The principles of safe design are to:
- Standardize
- Create independent checks
- Learn when things go wrong
Applied to hypertension control, standardization ensures blood pressure is measured correctly. If it’s not, independent checks will catch errors. Changing the process if mistakes occur closes the loop of safe design.
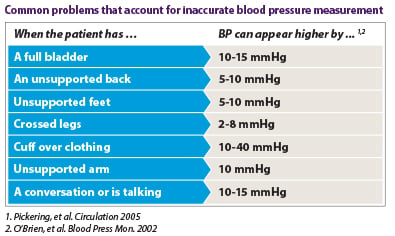
For example, if a patient’s feet aren’t flat on the floor or the patient’s arm and back aren’t properly supported, or the arm is not bare, there’s a chance that blood pressure measurement will give a falsely high reading. (See table below.) This could lead to a prescription for an unnecessary—and potentially harmful—medication. On the flip side, other factors can contribute to unidentified and untreated hypertension.
To help apply safe design principles to blood pressure control, the AMA and collaborators at Johns Hopkins are partnering with pilot practices in two locations to develop and test a set of evidence-based recommendations called “the M.A.P. for achieving optimal hypertension control”:
- Measuring blood pressure accurately every time it’s measured
- Acting rapidly to address high blood pressure readings
- Partnering with patients to promote self-management of high blood pressure
Lisa Cooper, MD, director of the Johns Hopkins Center to Eliminate Cardiovascular Health Disparities, and her team lead Project ReDCHiP (Reducing Disparities and Controlling Hypertension in Primary Care) and are leveraging their expertise in hypertension control improvement to help the larger AMA-JHM team integrate quality improvement and patient-centered care principles into the framework used by the pilot practice sites.
Another pilot program under the AMA’s Improving Health Outcomes initiative is working with physician practices to develop a model to create clinical-community linkages aimed at reducing the incidence of type 2 diabetes among patients with prediabetes.