AMA Update
4 potential causes of long COVID
Practice Management
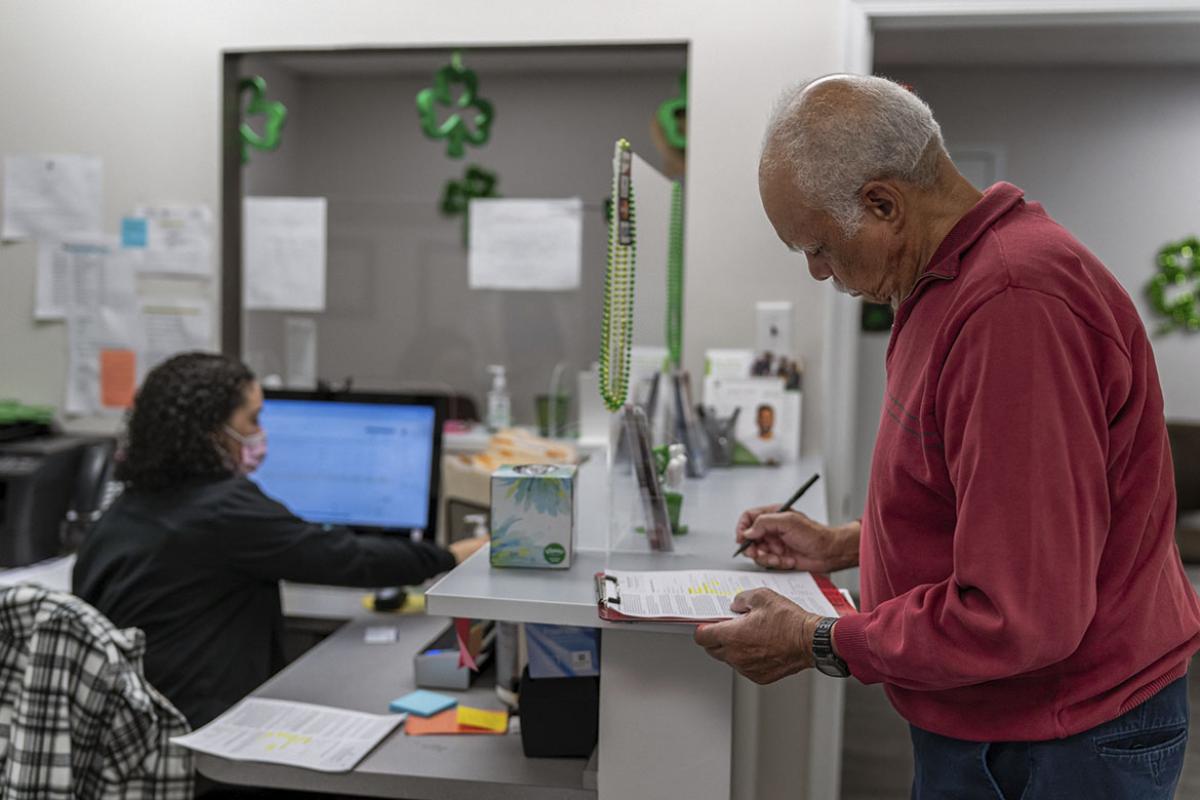
Change Healthcare outage leaves physician practices reeling
Health System Spotlight
RVs aren’t just for camping: Bringing the clinic to the community
Federal Advocacy
Health spending back to pre-COVID rates—but not for physicians
- What illnesses are going around? RSV, COVID-19, influenza, measles outbreak, plus avian flu news
- Akiko Iwasaki on what causes long COVID, brain fog, the Yale Paxlovid study and long COVID treatments
- Senior Physicians Section (SPS) Governing Council elections
- What doctors wish patients knew about the contagious norovirus
- Change Healthcare cyberattack
Free CME for Members
AMA Recovery Plan for America’s Physicians
About the recovery plan
You took care of the nation. It’s time for the nation to take care of you. It’s time to rebuild. And the AMA is ready.
Learn moreFixing prior authorization
We’re standing up to insurance companies to eliminate care delays, patient harm and practice hassles.
Learn moreReforming Medicare payment
The evidence is clear. The Medicare payment system is on an unsustainable path, threatening patients' access to physicians.
Learn more
Fighting scope creep
Patients deserve care led by physicians—the most highly educated, trained and skilled health care professionals.
Learn moreSupporting telehealth
The AMA is fighting for legislation to permanently fix the restrictions on telehealth coverage and payment.
Learn moreReducing physician burnout
We are focused on removing administrative burdens, providing real-world solutions and helping physicians rediscover the joy in health care.
Learn moreMember benefits: Exclusive savings & resources

6 reasons to join the AMA
By becoming a member, you can play a role in shaping the future of medicine while growing professionally, no matter where you are in your training and career.
Learn moreAuto & transportation
AMA membership makes you eligible for exceptional savings on a host of impressive Mercedes-Benz and Volvo vehicles.
Learn moreHome & lifestyle offers
Find and purchase a new home, refinance an existing mortgage or protect your home with professional monitoring.
Learn more
Med student membership
Find leadership and advocacy opportunities, get test prep, showcase your research, and take advantage of discounts and benefits designed just for you.
Learn moreLoans & financial services
Whether it's a home, student, resident or personal loan or insurance, AMA provides the information to align your finances, and prepare for your future.
Learn moreAMA Annual Meeting
Event InformationAnnual Meeting of the House of Delegates
June 7-12, 2024
Member Groups (Sections) Meetings
June 6-7, 2024
Annual Meeting of the House of Delegates
June 7-12, 2024
Future HOD Meeting Dates
More InfoAMA Morning Rounds
Get your daily dose of medical news
The biggest stories in medicine and public health delivered right to your inbox.