Disclaimer: Information provided by the AMA contained within this Quick Guide is for medical coding guidance purposes only. It does not (i) supersede or replace the AMA’s Current Procedural Terminology (CPT®) manual (“CPT Manual”) or other coding authority, (ii) constitute clinical advice, (iii) address or dictate payer coverage or reimbursement policy, and (iv) substitute for the professional judgement of the practitioner performing a procedure, who remains responsible for correct coding.
CPT © Copyright 2023 American Medical Association. All rights reserved. AMA and CPT are registered trademarks of the American Medical Association. More information can be found on our CPT site.
The policy and payment landscape around telehealth and telemedicine remains complex, and as the public health emergency expires, there will be some uncertainty to navigate related to telehealth policy, coding and payment. The AMA’s Advocacy team will continue to summarize the latest updates in federal and state policy.
What to expect post PHE
The following outlines key policies or actions taken during the COVID-19 pandemic that have been extended past the end of the COVID-19 Public Health Emergency (PHE) either by CMS or through the Consolidated Appropriations Act (CAA) of 2023:
- Category 3 telehealth services will be covered through 2023.
- Nonfacility payment rates for telehealth services will remain the same through 2023 (physician offices are defined by Medicare as “nonfacility” setting, so this means telehealth payments will remain the same as in-person through 2023.
- Direct supervision may continue to be provided virtually through 2023.
- Geographic and originating site restrictions on Medicare telehealth services are waived beginning the day of the Public Health Emergency through December 31, 2024.
- The in-person requirement on Medicare telemental health services is delayed until on or after January 1, 2025.
- Medicare coverage and payment of audio only services will continue through December 31, 2024.
- The acute hospital care at home model is extended through 2024.RPM can permanently be used for both chronic and acute conditions.
- The ability of Opioid Treatment Programs (OTPs) to provide patient counseling and therapy by phone is permanent.
- Recertification of eligibility for hospice care can continue to be conducted via telehealth.
- Rural ERs can be originating sites.
- An in-person visit will not be required for a patient to be eligible for behavioral health services via telehealth through December 31, 2024.
- Codes for reimbursement for audio-only telebehavioral health services which will only be covered through December 31, 2024.
There are also several policy changes and updates to be aware of moving forward including:
- CMS decided to continue paying for all of the codes on the telehealth list that were scheduled to stop 151 days after the PHE through the end of 2023, with future policy to be determined in future rulemaking, likely the 2024 Medicare physician payment regulation.
- The Drug Enforcement Administration extended its PHE policies on prescribing controlled substances based on telehealth visits for six months after the PHE end until Nov. 11, 2023, to provide time to develop new regulations.
- How and when OCR will start to enforce and imposed penalties on covered health care providers for noncompliance with the requirements of the HIPAA Rules in connection with the provision of telehealth using non-public facing audio or video remote communication technologies.
- The Office for Civil Rights (OCR) is providing a 90-day transition period (PDF) for physicians to come into compliance with the HIPAA Rules regarding telehealth. OCR is responsible for enforcing certain regulations to protect the privacy and security of protected health information, collectively known as the HIPAA Rules. At the beginning of the COVID-19 public health emergency (PHE), the AMA urged policymakers to make it easier for physicians to utilize telehealth in their practice. This included using remote communication technologies for virtual office visits. HIPAA requires that physicians meet certain privacy and security requirements when using remote communication technologies. Responding to AMA advocacy, OCR exercised enforcement discretion (PDF) and did not enforce penalties for physicians who could not or did not meet certain HIPAA requirements.
- On May 11, the COVID-19 PHE will end and sunset several PHE-related federal policies. The AMA has advocated for additional time for physicians to come into compliance with HIPAA. In response to AMA advocacy, OCR is providing a transition period beginning on May 12 through Aug. 9. OCR recognizes that many physicians began using remote communication technologies for telehealth for the first time during the COVID-19 PHE and need additional time to come into compliance. Therefore, physicians may use this transition period, as necessary, to adjust their telehealth practices to come into compliance, such as by choosing a telehealth technology vendor that will enter into a business associate agreement and comply with applicable requirements of the HIPAA Rules. OCR will continue to exercise its enforcement discretion and will not impose penalties on physicians for noncompliance with the HIPAA Rules during the 90-calendar day transition period.
- RPM services were able to be provided to new and established patients during PHE, but following the end of the PHE, there must be an established relationship.
- During PHE, RPM could be reported for as few as two days for COVID patients, but this reverts back to 16 days after PHE.
- CMS has not been enforcing LCDs on therapeutic continuous glucose monitors during the PHE to allow people with COVID and diabetes to monitor glucose and adjust insulin at home. This waiver ends with the PHE.
- CMS decided to not enforce frequency limits for the rest of 2023 and to address them in future rulemaking.
- CMS suspended plans to require physicians who provide services from their home to report their home address on their Medicare enrollment through the end of 2023 and will address in future rulemaking.
- CMS has agreed to allow MIPS-eligible physicians to request hardship waivers for performance year 2023.
- Telehealth services provided by Rural Health Clinics (RHCs) and Federally Qualified Healthcare Centers (FQHCs) can be distant site providers for behavioral health and non-behavioral telehealth services.
- Select non-behavioral telehealth services can be provided via audio-only options.
- Laws about physician licensure will continue to defer to state law―no federal policy.
- In response to AMA advocacy, CMS agreed to continue to allow teaching physicians to provide virtual supervision of residents through 2023 and will address future policy in future rulemaking.
See the full list of authorized telehealth services in the Calendar Year 2023 Medicare Physician Fee Schedule.
Policy and payment considerations
Here are some additional key policy and payment considerations to keep in mind:
- Ensure that you provide services per your state laws and regulations. As part of emergency declarations, many governors relaxed state laws and regulations related to the provision of telehealth services during the pandemic. States varied on whether these changes were tied to the state PHE or federal PHE, as some of these flexibilities are no longer available. For up to date information in your state, please contact your state department of health or state medical association.
- Licensure:
- There are no additional requirements if you are licensed in the state where the patient is located.
- If you are not licensed in the state where the patient is located there are several options for physicians to obtain a license or meet the state’s licensure requirements. These options vary by state:
- Interstate Medical Licensure Compact
- Licensure by endorsement
- Special purpose telehealth registry or license
- Exceptions to in-state licensure requirements
- CMS has issued the following waiver for Medicare patients (PDF): Temporarily waive requirements that out-of-state clinicians be licensed in the state where they are providing services when they are licensed in another state. Physicians are still bound by their state licensing requirements (CMS FAQs [PDF]).
- The Federation of State Medical Boards (FSMB) is tracking executive orders related to licensure. Stay up to date on the FSMB website.
- The AMA has created the following issue brief: Telehealth licensure: Emerging state models of physician licensure flexibility for telehealth (PDF).
- If you are not licensed in the state where the patient is located there are several options for physicians to obtain a license or meet the state’s licensure requirements. These options vary by state:
- There are no additional requirements if you are licensed in the state where the patient is located.
- CMS expanded access to telemedicine services for all Medicare beneficiaries during the COVID-19 Public Health Emergency. CMS will continue to allow the use of telehealth services until December 31, 2024. In addition to existing coverage for originating sites including physician offices, skilled nursing facilities and hospitals, Medicare will now pay for telehealth services furnished in any healthcare facility and in the home.
AMA provides a resource of COVID-19 flexibilities (PDF) that will end with the PHE.
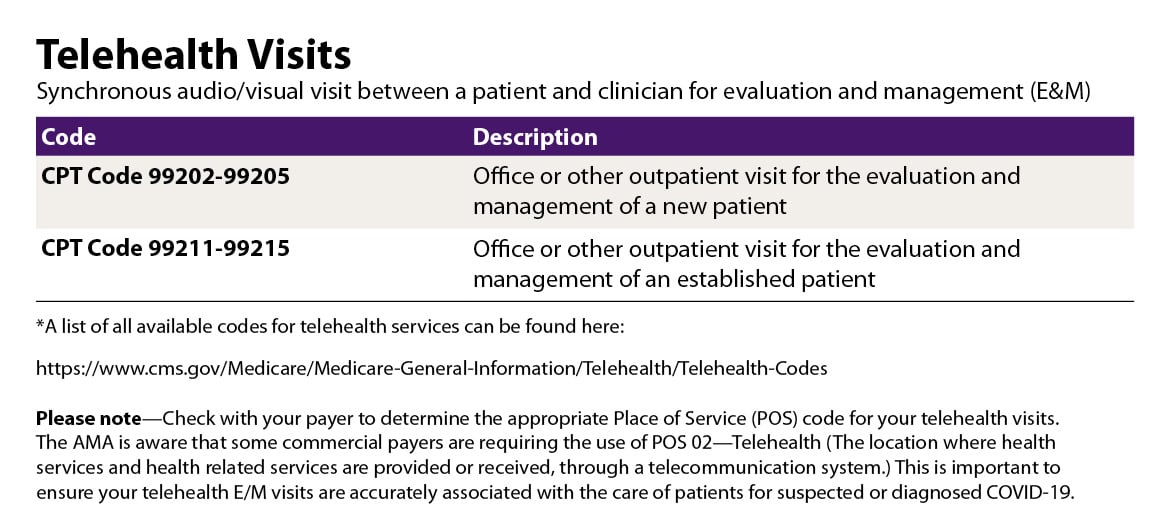
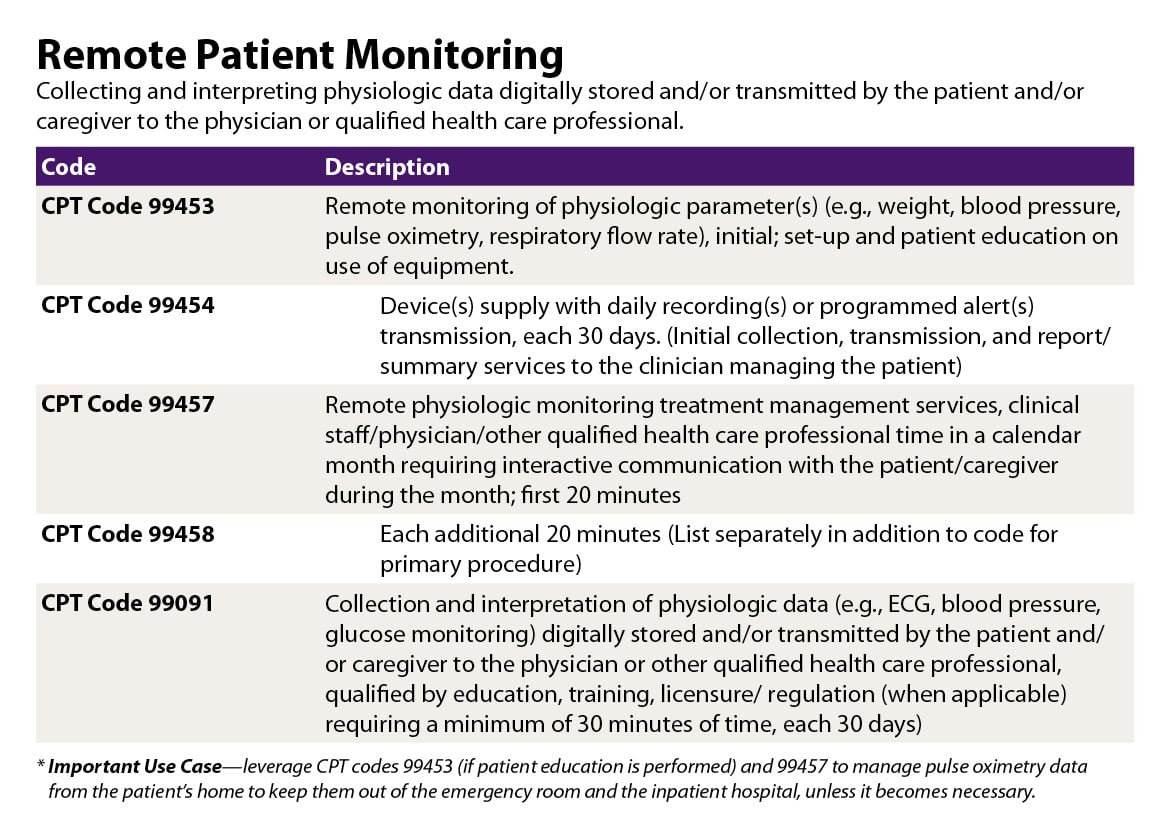
Telemedicine CPT codes
Common CPT codes for telemedicine services are listed below.
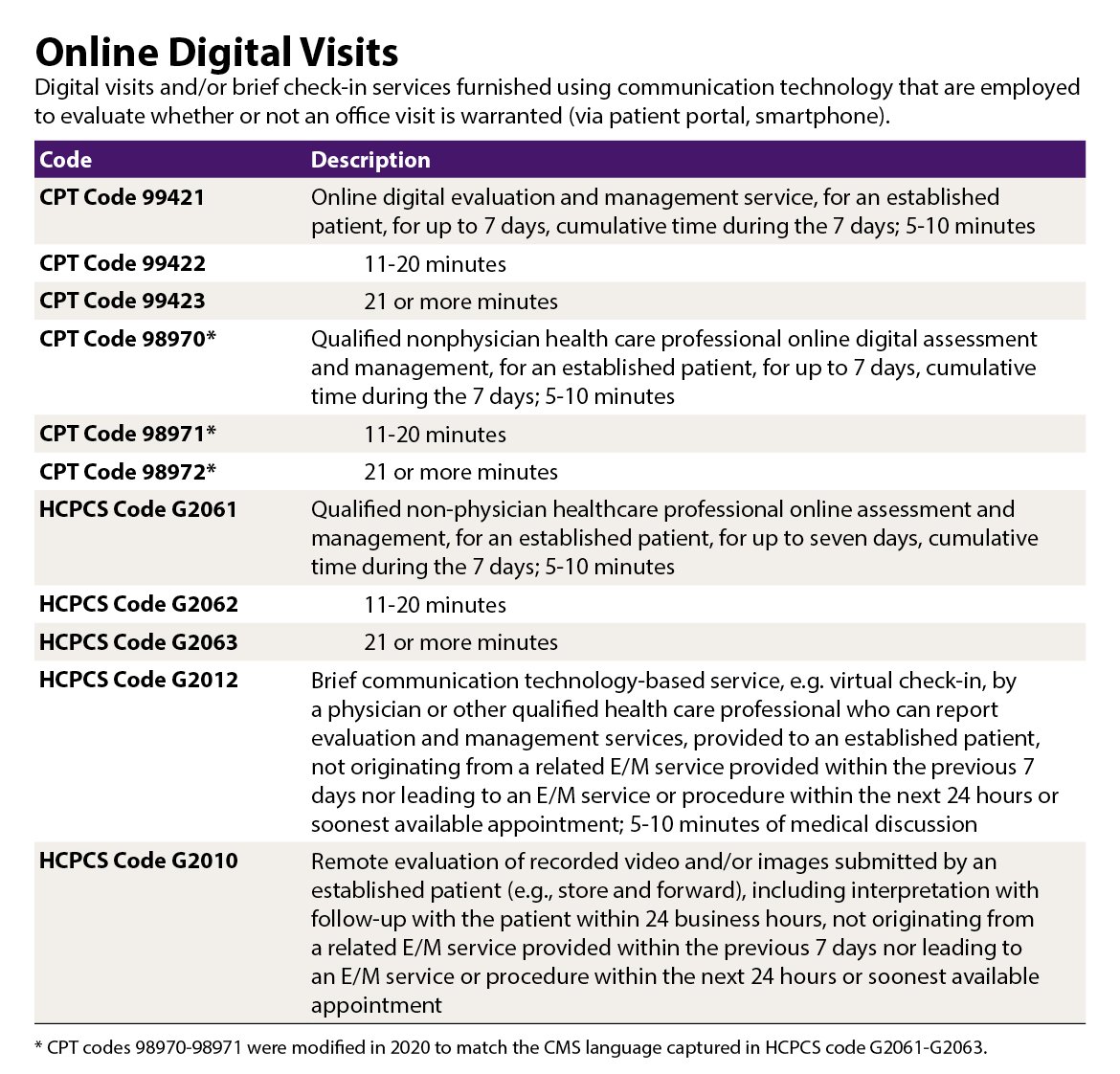
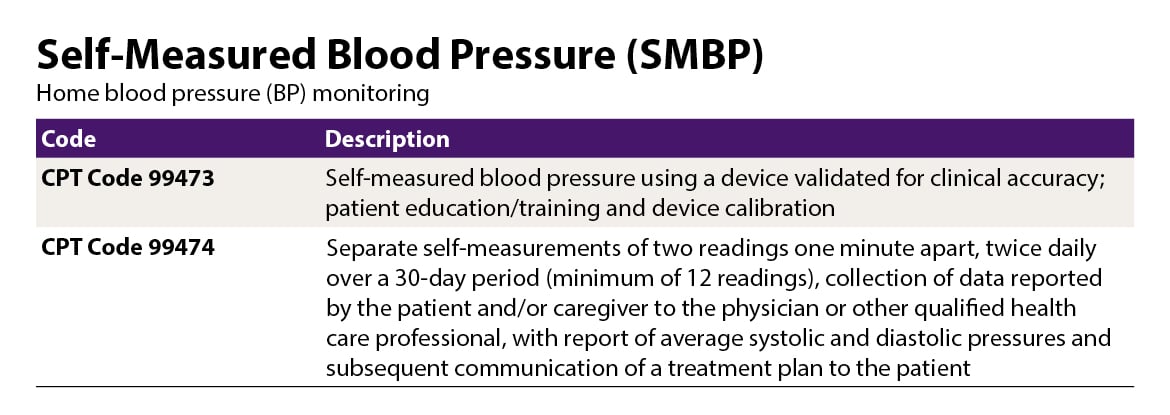
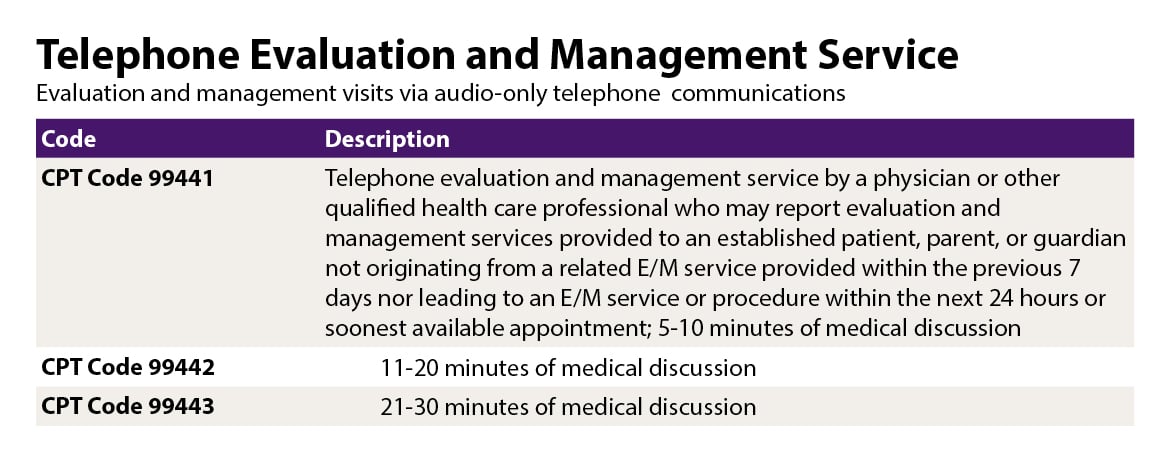
The tables on this page give common CPT codes for telemedicine services; other codes may be needed.
- CPT Codes: 99091, 98970, 98971, 98872, 99201, 99202, 99203, 99204, 99205, 99211, 99212, 99213, 99214, 99215, 99421, 99422, 99423, 99441, 99442, 99443, 99453, 99454, 99457, 99458, 99473 and 99474
- HCPCS Codes: G2061, G2062, G2063, G2012 and G2010