Editor’s note: In an April 24 statement, Dr. Ehrenfeld commended CMS for finalizing “historic rules that will strengthen access to care and improve health outcomes for Medicaid patients across fee-for-service and managed-care delivery systems.”
The Biden administration has recently taken some positive steps to help more Americans gain access to high-quality health insurance coverage.
First is a newly finalized rule governing short-term, limited-duration insurance that closes loopholes and protects people from misleading marketing tactics by requiring health insurers to be up front with consumers about coverage so they can better distinguish such plans from more comprehensive coverage.
The rule also reinstates a previous limit on these plans to no more than four months, reversing the up to three-year allowed under the previous administration. In 2018, the AMA opposed (PDF) the definitional changes to these plans.
The Biden administration action also bars the same carrier from issuing multiple short-term plans to the same policyholder within a 12-month period, a tactic known as “stacking.” That is a change the AMA supported in comments (PDF) to the proposed rule last September.
Unlike most health insurance offerings, short-term plans are not subject to the Affordable Care Act’s consumer protections such as protections against discrimination for preexisting conditions.
In a statement, AMA President Jesse M. Ehrenfeld, MD, MPH, hailed the administration for “cracking down on junk insurance.”
“These short-term policies are often marketed and sold in a misleading and deceptive manner, leading consumers to confuse them for comprehensive insurance,” Dr. Ehrenfeld noted. “Under the new rule, health insurance companies must clearly state what consumers are buying so they are not left with onerous medical bills after accessing health care. The changes laid out in today’s rule will lessen risks to consumers, promote transparency, expand patient protections and help to stabilize the market.”
He added that “while these policies of short duration may be less expensive, they also provide fewer benefits and do not have to comply with critical consumer protections of the Affordable Care Act (ACA). For too long, companies have used deceptive marketing to trick people into buying health plans that discriminate based on pre-existing conditions while providing little or no coverage.”
Visit AMA Advocacy in Action to find out what’s at stake in covering the uninsured and other advocacy priorities the AMA is actively working on.
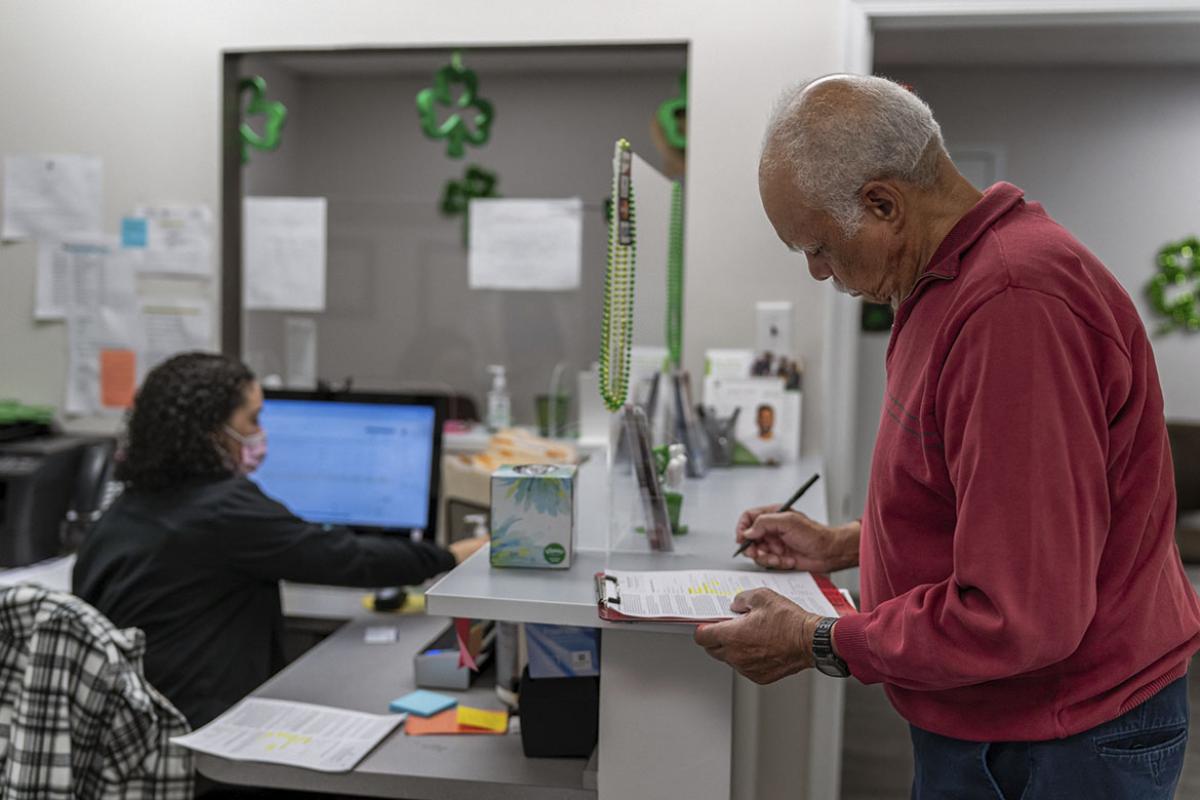
Easing Medicaid, CHIP enrollment
The Centers for Medicare & Medicaid Services (CMS), meanwhile, also took steps to streamline enrollment in Medicaid and the Children’s Health Insurance Program (CHIP). The rule, also finalized in March, “will simplify the enrollment process and reduce other enrollment barriers for individuals who are eligible for Medicaid and CHIP,” Dr. Ehrenfeld said.
“Complex applications and duplicative requests for documentation disproportionately impact marginalized and minoritized individuals,” he added. “No one should experience gaps in coverage due to burdensome administrative processes. Even brief gaps in coverage can be extremely disruptive for medical treatments and medication adherence.”
Among other things, this CMS action establishes protections for children by:
- Eliminating annual and lifetime limits on children’s coverage in CHIP.
- Ending the practice of locking children out of CHIP coverage if a family is unable to pay premiums.
- Eliminating waiting periods for CHIP coverage.
- Improving the transfer of children seamlessly from Medicaid to CHIP when a family’s income rises.
The rule also protects older adults and people with disabilities by:
- Eliminating in-person interview requirements.
- Using auto-populated renewal forms.
- Barring renewals from happening more than once annually.
- Requiring states to use existing electronic data to update contact information and verify eligibility without requiring additional verification of assets.
In previous comments (PDF), the AMA expressed support for the now-finalized changes.
The Biden administration also separately extended a temporary special enrollment period to help people no longer eligible for Medicaid or CHIP transition to marketplace coverage. Nearly 20 million Medicaid enrollees across the country had been disenrolled as of March 26, according to KFF.
“Together, these actions will strengthen patient protections and close coverage gaps, helping millions of Americans gain or keep coverage and access care,” Dr. Ehrenfeld said.
In a related action, CMS in April finalized another rule making it easier for patients with low incomes to enroll in ACA Marketplace coverage, expanding consumer protections, and setting distance standards for in-network appointments and network adequacy standards for the time. The AMA supported these changes in comments (PDF) to the agency in January.