Contents
Catch up with the news and other key moments from the AMA House of Delegates’ virtual meeting. The November 2021 AMA Special Meeting ran Nov. 12–16.
For a briefer rundown, check out this list of our top 10 stories from the Special Meeting.
The 2022 AMA Annual Meeting is scheduled for June 11–15 next year at the Hyatt Regency Chicago. Whether a June 2022 AMA House of Delegates meeting happens virtually or in person is subject to the evolving conditions of the COVID-19 pandemic.
Wednesday, Nov. 17
Enable real-time Rx benefit info to boost truth in drug pricing
A standardized real-time prescription benefit (RTPB) tool embedded in EHRs would help patients and physicians make cost-informed decisions on prescription drugs while improving price transparency and medication adherence, according to an AMA Council on Medical Service report adopted at the Special Meeting.
However, “a standard is needed to progress beyond the current proprietary and incomplete RTPB technology landscape and allow all physicians access through any EHR to any patient’s specific benefit information,” the council report says, while noting that the technology is “not a panacea that can solve the much broader problem of prescription drug cost transparency in all contexts.”
Learn how the AMA will support efforts to publish such an RTPB standard to close the information gaps among patients, doctors, payers and pharmacies.
Make menstrual products widely available at no cost
It’s estimated that a typical woman spends over $1,700 on menstrual products during her lifetime, making the products unaffordable for two-thirds of people with low incomes in the U.S. according to a resolution presented at the Special Meeting by the AMA Medical Student Section.
To improve access to menstrual products, the House of Delegates adopted new policy to:
- Recognize the adverse physical and mental health consequences of limited access to menstrual products for school-aged individuals.
- Support the inclusion of medically necessary hygiene products, including but not limited to, menstrual hygiene products and diapers, within the benefits covered by appropriate public assistance programs.
- Encourage public and private institutions as well as places of work and education to provide free, readily available menstrual care products to workers, patrons and students.
“Without proper hygiene products, women sustain infections, injuries or embarrassment. Women report high rates of having had to miss work since menstrual products are not available publicly, and girls report high rates of having had to miss school for the same reason,” said AMA Trustee Willie Underwood III, MD, MSc, MPH.
“Moving policy in this direction will combat gender inequities by making hygiene products available in public spaces, including schools, and incorporating these products in supplemental nutrition programs,” Dr. Underwood added.
The House of Delegates also amended existing policy to “encourage the American National Standards Institute, the Occupational Safety and Health Administration and other relevant stakeholders to establish and enforce a standard of practice for providing free, readily available menstrual care products to meet the needs of workers.”
Lastly, delegates directed the AMA to advocate federal legislation and “work with state medical societies to increase access to menstrual hygiene products, especially for recipients of public assistance.”
Collaboration needed to end spread of public health misinformation
There is ongoing concern over the harmful effects of disinformation being disseminated by a small number of health professionals. Such falsehoods have been directly linked to vaccine hesitancy and have also contributed to the disregard for proper prevention practices such as mask-wearing, physical distancing and handwashing, says a resolution from the AMA Young Physicians Section (AMA-YPS) presented at the Special Meeting.
“Physicians are among the most trusted source of information and advice for patients and the public at large, which is why it’s so dangerous when a physician or other health care professional spreads disinformation,” said AMA Trustee Jesse M. Ehrenfeld, MD, MPH.
“While disinformation has run rampant during the COVID-19 pandemic, we know unscientific claims are being made about other health conditions and other public health initiatives are being undermined,” Dr. Ehrenfeld added. “We are committed to doing everything we can to stop the spread of disinformation and providing accurate, evidence-based information—the lives of our patients and the public depend on it.”
Learn more about how the AMA will fight against misinformation disseminated by health professionals.
Tuesday, Nov. 16
Sweeping plan outlined to address maternal health care inequities
Improving maternal health care among people from historically marginalized communities means raising awareness about the health impacts of racial and ethnic inequities, extending public health care programs to cover new mothers for 12 months after the end of pregnancy, and investing in research and outreach, according to a joint report from the AMA Council on Medical Service and the AMA Council on Science and Public Health.
According to the joint report, “two foundational first steps are expanding access to affordable health insurance and eliminating racial and ethnic inequities in care and outcomes.” For example, Black women are much more likely than white women to die from pregnancy-related causes or experience severe maternal morbidity.
“The AMA is committed to being a leader on maternal mortality prevention, and the nation’s physicians have charged the AMA to prioritize the elimination of racial and ethnic inequalities in maternal health care while increasing access to affordable health insurance for new mothers,” said AMA Immediate Past President Susan R. Bailey, MD. “As a first step, the AMA acknowledges the roles that structural racism and bias play in negatively impacting health care, including maternity care.”
Read more about the delegates' actions to promote maternal health care equity.
Time for payers to expand home and community-based services
Home and community-based services (HCBS) offer a safer alternative for patients with certain conditions, avoiding the risks that come with inpatient admission and care. That is especially true amid the COVID-19 pandemic. An AMA Council on Medical Service report adopted at the Special Meeting pushes for state and federal reforms to strengthen financing of long-term services and supports (LTSS) for home and community-based services.
“As the U.S. population ages, beneficiary preferences evolve, and demographic shifts continue, HCBS provides a desirable and cost-effective way of delivering LTSS to seniors and those with disabilities,” says the council’s report says.
To help advance HCBS, the AMA House of Delegates adopted new policy to support:
- Federal funding for payment rates that promote access and greater use of HCBS.
- Policies that help train, retain, and develop an adequate HCBS workforce.
- Efforts to simplify state plan amendments and Medicaid waivers to allow additional state flexibility to offer HCBS.
- That Medicaid’s Money Follows the Person demonstration program be extended or made permanent.
- Cross-agency and federal-state strategies that can help improve coordination among HCBS programs and streamline funding and the provision of services.
- HCBS programs tracking protocols and outcomes to make meaningful comparisons across states and identify best practices.
- That the Centers for Medicare & Medicaid Services and private insurers extend flexibility to implement innovative programs including but not limited to hospital-at-home programs.
Teens need privacy, confidentiality during telehealth visits
The AMA has long recognized the importance of adolescents having privacy and confidentiality to discuss sensitive issues with physicians without a parent present. The increased use of telehealth doesn’t change the importance of that need, but does present new challenges in providing confidential care, according to a resolution from the Michigan delegation that was adopted at the AMA Special Meeting.
For example, it can be challenging for a teenager to find a quiet and private space in the home that is separate from other family members and allows them to discuss sensitive topics without the fear of someone overhearing the conversation.
“Telehealth utilization has skyrocketed during the COVID-19 pandemic, providing opportunities for ongoing patient care,” said AMA Trustee Willie Underwood III, MD, MSc, MPH. “We must keep in mind that adolescents need privacy to engage in confidential patient-physician communications. Physicians, patients and parents all need guidance on how best to address confidentiality concerns.”
With those concerns in mind, the House of Delegates amended existing policy encouraging physicians to:
- Recognize the unique confidentiality concerns of adolescents and their parents associated with telehealth visits.
- Offer—in a telehealth setting—a separate examination and counseling apart from others to ensure that the adolescent is in a private space.
Include medical cannabis license certification in PDMPs
Physicians are better able to manage their patients’ care when they have access to all relevant information, including a patient’s cannabis use that is included in a prescription drug-monitoring program (PDMP). But doctors are concerned that adding more information to a PDMP without the right safeguards to ensure patient privacy could be detrimental, according to an AMA Board of Trustees report adopted at the Special Meeting.
“If a patient has been certified as having a medical condition qualifying that patient for medical cannabis, that information should be available to other physicians,” said AMA Trustee Thomas J. Madejski, MD. “But it’s equally important to protect the privacy of medical information in a PDMP from law enforcement and others. That’s why it’s best that PDMPs contain limited information about a patient’s medical cannabis use.”
The House of Delegates took action calling for the AMA to:
- Support efforts to include medical cannabis license certification in states’ PDMPs when consistent with AMA principles safeguarding patient privacy and confidentiality.
- Continue monitoring state legislation relating to the inclusion of cannabis and related information in state PDMPs.
- Review existing state laws that require information about medical cannabis to be shared with or entered into a state PDMP. The review should address impacts on patients, physicians and availability of information including types, forms, THC concentration, quantity, recommended usage, and other medical cannabis details that may be available from a dispensary.
Protect future doctors’ access to abortion education, training
About one-quarter of American women have an abortion by age 25, yet medical education on the procedure lags behind its prevalence, according to an AMA Medical Student Section resolution presented at the AMA Special Meeting.
To help protect access to abortion education and training, delegates modified AMA policy to:
- Support the education of medical students, residents and young physicians about the need for physicians who provide termination of pregnancy services, the medical and public health importance of access to safe termination of pregnancy, and the medical, ethical, legal and psychological principles associated with termination of pregnancy.
- Support the availability of abortion education and exposure to procedures for termination of pregnancy, including medication abortions, for medical students and resident/fellow physicians and opposes efforts to interfere with or restrict the availability of this education and training.
- Encourage the Accreditation Council for Graduate Medical Education to consistently enforce compliance with the standardization of abortion training opportunities as per the requirements set forth by the Review Committee for Obstetrics and Gynecology and the American College of Obstetricians and Gynecologists’ recommendations.
“The AMA recognizes the value of an immersive and comprehensive educational experience for residents and medical students in the provision of abortion care—while still respecting personal, religious and moral convictions of all trainees,” said AMA President Gerald E. Harmon, MD. “Protecting access to such training equips the next generation of physicians with the crucial skills needed to ensure our patients have access to their choice of safe, high-quality reproductive care. which is essential for improving the health of the nation.”
AMA seeks more help for medical students, residents with disabilities
Nearly one in 20 medical students presents with a disability, according to 2019 data. That number has been on the rise in recent years and represents an opportunity to create a more diverse physician workforce that can introduce new approaches to care.
“The AMA strongly supports efforts to increase the diversity of our future physician workforce,” said AMA Trustee Drayton Charles Harvey, fifth-year MD-PhD student. “By examining the roadblocks that medical students and trainees with disabilities often face, we can prioritize inclusion, eliminate stigmatization, and change the medical education experience.”
Read more about delegates' actions to remove barriers and refocus on student and trainee abilities, not limitations.
How policing can benefit from medicine’s evidence-based approach
Both police officers and physicians often face high-pressure situations in which they must make time-sensitive, life-or-death decisions and “it may benefit law enforcement to borrow some of the strategies and practices that the medical profession uses to ensure that its members provide safe and effective care,” says an AMA Board of Trustees report whose recommendations were adopted at the Special Meeting.
“The AMA is strongly invested in the betterment of public health and remains committed to advocating for actionable reform to eliminate excessive police violence in historically marginalized communities,” said AMA Trustee Willie Underwood III, MD, MS, MPH. “We value the opportunity to contribute the scope of the AMA’s expertise to the national conversation on policing—especially as it relates to improving the health of our patients and the overall health of the nation.”
Read more about the lessons that police could draw from physicians on how to scrutinize and prevent unwanted outcomes.
MDs, DOs should decide who gets medical vaccine exemptions
The COVID-19 pandemic makes it even more timely and urgent that only licensed physicians be allowed to decide who qualifies for vaccine exemptions for medical reasons, says an AMA Medical Student Section resolution adopted at the Special Meeting.
Today, all jurisdictions offer medical contraindication exemptions to vaccine mandates, but the process differs from state to state. Some states allow any health professional to supply a patient with a medical exemption. That could allow, for example, naturopaths to provide exemptions, the resolution says. Recent surveys have found that at most only 20% of naturopaths actively recommend vaccination and as many as 7% actively advise against vaccination.
To protect public health, the House of Delegates amended existing policy to “limit medical vaccine exemption authority to only licensed physicians.”
“Vaccine hesitancy has played an unfortunate role in extending the COVID-19 public emergency. Failing to get vaccinated has resulted in tragic and unnecessary deaths. To protect everyone, we must be sure that a trained, licensed physician is making the judgment on whether a person actually warrants an exemption,” said AMA Trustee Willie Underwood III, MD, MSc, MPH.
“State policymakers need to limit the definition to physicians who have the training necessary to recognize a medical condition that prevents a patient from receiving a vaccine,” Dr. Underwood added. “We shouldn’t jeopardize public health by listening to unlicensed and untrained providers.”
Protect sensitive individual data at risk from DTC genetic tests
Use of direct-to-consumer (DTC) genetic tests has grown exponentially over the past decade, with an estimated 100 million individuals expected to have undergone the testing by the year’s end, according to an AMA Board of Trustees report adopted at the Special Meeting.
And physicians say more needs to be done to ensure there are safeguards in place for people to protect their sensitive information.
“People curious about their ancestry shouldn’t be worried that the data extracted from saliva will be shared,” said Thomas J. Madejski, MD, a geriatrician and AMA trustee. “This can have serious consequences, and again highlights the need to demand privacy for health care records, even seemingly innocuous ones.”
Read more about the AMA's call for new privacy standards to govern this burgeoning market.
Add rural medicine exposure in training to boost country doctors
One of in five Americans lives in a rural community. Those areas face physician shortages across medical specialties. While 15% of the U.S. population lives in rural areas, only 12% of primary care physicians work in rural areas, and that share dips to only 8% in all other specialties.
“For the nearly 60 million people who live in rural communities across America, persistent inequities continue to place barriers on access to medical care – resulting in devastatingly higher rates of mortality and preventable hospitalizations for this patient population,” said AMA Board of Trustees Member Scott Ferguson, MD. “There is a clear, urgent need for more physicians to serve in rural America to help close existing gaps in patient care. The AMA is dedicated to addressing the root causes of health inequities for the rural patient population, and this policy is one step closer to removing those obstacles to care and achieving optimal health for all.”
Read more about the House of Delegates' actions to proactively address the physician shortage in rural areas.
Stop payers from wrongly charging EFT fees
Federal laws require health insurers to offer network physicians a no-charge option for electronic funds transfer (EFT), but some health insurers and their vendors are inappropriately charging for those transactions, says a resolution adopted at the AMA Special Meeting.
To fight those practices, the House of Delegates directed the AMA to:
- Forcefully advocate that the Centers for Medicare & Medicaid Services (CMS) investigate all valid allegations of HIPAA administrative-simplification requirements thoroughly and offers transparency in its processes and decisions as required by the Administrative Procedure Act.
- Forcefully advocate that the CMS resolve all complaints related to the non-compliant payment methods including opt-out virtual credit cards, charging processing fees for electronic claims and other illegal EFT fees.
- Communicate its strong disapproval of the failure by the CMS Office of Burden Reduction to effectively enforce the HIPAA administrative-simplification requirements as required by the law and its failure to impose financial penalties for noncompliance by health plans.
- Through legislation, regulation or other appropriate means, advocate for the prohibition of health insurers charging physicians and other providers to process claims and make payments.
Give physicians access to patient billing, medical records
Doctors can be exposed to severe penalties if they are unable to access billing records and associated medical records to monitor their compliance with federal and state laws, notes an AMA Board of Trustees report adopted at the Special Meeting.
To ensure that physicians are able to monitor and comply with billing done under their name, the House of Delegates directed the AMA to advocate:
- That licensed physicians have unrestricted access to all their patients’ billing records and associated medical records during employment or while under contract to provide medical or health care items or services. The records should include any billing records submitted under the physician’s name, regardless of whether the physician directly provided the item or service.
- That, where physician possession of all his or her billing records is not already required by state law, the employment or other contractual arrangement between a physician and entity submitting claims on behalf of the physician should specify that the physician is entitled to copies of his or her billing records subsequent to the termination of employment or contractual arrangement, when such records are necessary for the physician’s defense in malpractice actions, administrative investigations, or other proceedings against the physician.
- Legislation or regulation to eliminate contractual language that bars or limits the treating physician’s access to his or her billing records and associated medical records, such as treating these records as trade secrets or proprietary.
Pursue harm-reduction approach to prevent drug overdose deaths
The COVID-19 pandemic has rightly grabbed the public health spotlight around the globe. But the drug-overdose epidemic remains a persistent challenge, one that has been exacerbated by the pandemic.
Making matters worse, chemical adulterants such as synthetic opioids are increasing in prevalence in nonopioid drugs. Yet current paraphernalia laws limit harm reduction for people who use injection drugs, says an AMA Medical Student Section resolution presented during the Special Meeting.
“Over the past decade, mitigation efforts like syringe service programs have effectively promoted safe use and recovery for people who inject drugs,” said AMA Immediate Past Board Chair Russel W.H. Kridel, MD. “This policy builds on those successful efforts and seeks to break down barriers to better address the ongoing tragedy of the drug-related overdose crisis.”
Recognizing the changing nature of drug-overdose epidemic and the need to emphasize harm reduction, the House of Delegates modified existing policy to help save lives.
Among other things, the AMA will advocate and encourage state and county medical societies to advocate for harm-reduction policies that provide civil and criminal immunity for the use of “drug paraphernalia” that is designed for harm reduction from drug use including but not limited to drug-contamination testing and injection-drug preparation, use and disposal supplies.
Skin-tone diversity matters in dermatologic training, diagnosis
Using the skin tones of people from historically marginalized racial and ethnic groups in training materials has been shown to help achieve equitable diagnostic outcomes.
Yet about 75% of dermatological imagery in medical textbooks represent individuals with lighter skin tones. Core dermatology textbooks used to educate medical students, residents, dermatologists and physicians in other specialties also have limited representations of skin color, says a resolution the AMA Medical Student Section presented at the Special Meeting.
“There is a significant gap in training and education with important downstream impacts on patient populations,” said AMA Immediate Past Board Chair Russell W.H. Kridel, MD. “By bolstering diversity in imaging and educational materials, the chance for early detection of skin cancer and other dermatologic pathologies is greatly increased among populations with darker skin tones.”
To address the issue, the House of Delegates adopted new policy that encourages “comprehensive, inclusive and equitable representation of a diverse range of skin tones in all dermatologic and other relevant medical educational resources for medical students, physicians, nonphysician health care providers and patients.”
Save lives by protecting all workers from heat exposure
Prolonged exposure to heat can cause exhaustion, cramps, stroke and death. It can also exacerbate preexisting conditions, including respiratory, cerebral and cardiovascular diseases.
Despite the fact that heat-related deaths are preventable, nearly 700 people succumb to extreme heat each year in the U.S. And since 2010, Hispanic people have accounted for one-third of all heat fatalities while representing only 17% of the U.S. workforce, according to a resolution presented by the Washington state delegation at the AMA Special Meeting.
“Every person should have the right to work in an environment that’s safe and free from the dangers of extreme heat,” said AMA Immediate Past Board Chair Russell W.H. Kridel, MD. “We believe that better federal heat-specific injury protections are needed to protect all workers from heat-related illness, injury and death, whether working inside or outside.”
To help prevent heat-related deaths and injuries, the AMA House of Delegates adopted new policy to:
- Support policy change at the federal level via legislation or administrative rule changes by the Occupational Safety and Health Administration (OSHA) that would require that workers receive health educational materials about prevention and recognition of heat exhaustion and heat-exposure injury that is in the worker's primary language.
- Recognize there are particular medical conditions and medications, including but not limited to psychotropics, which increase an individual’s vulnerability to the negative impacts of heat and sun exposure and advocate for recognition of this, as well as additional protections as part of any guidelines, legislation or other policies.
Delegates also directed the AMA to:
- Advocate that all outdoor workers to have access to preventive cool-down rest periods in shaded, ventilated or cooled areas for prevention of injury from sun exposure and heat injury, as well as appropriate access to emergency services when signs and symptoms of heat exposure injury appear.
- Work with the U.S. Department of Labor, OSHA and other appropriate federal stakeholders to develop and enforce evidence-based policies, guidelines and protections against heat injury for outdoor workers independent of legal status.
Equity for grads of LCME-accredited Puerto Rican medical schools
There are four allopathic medical schools accredited by the Liaison Committee on Medical Education (LCME) in Puerto Rico. Most Puerto Rican medical students attending those schools are U.S. citizens. Yet there are numerous barriers in the procurement of away rotations and residency program spots for those students, according to an AMA Medical Student Section resolution presented at the Special Meeting.
To help address those barriers, the House of Delegates directed the AMA to work with the LCME, as well as “the Middle States Commission on Higher Education (MSCHE), and Association of American Medical Colleges (AAMC) to inform residency and fellowship program directors and training programs in the United States that graduates of medical schools in Puerto Rico that are accredited by the LCME and MSCHE are U.S. medical school graduates.”
Delegates also adopted new policy to “support policies that ensure equity and parity in the undergraduate and graduate educational and professional opportunities available to medical students and graduates from all LCME- and Commission on Osteopathic College Accreditation (COCA)-accredited medical schools.”
Clarity needed on board scores’ use for residency applications
By May 2022, both the United States Medical Licensing Examination (USMLE) Step 1 exam and Comprehensive Osteopathic Medical Licensing Examination of the United States (COMLEX USA) Level 1 will have moved to pass-fail scoring from a prior numerical format.
That creates the potential for upcoming residency selection cycles in which some candidates will have a numerical exam score and others will have only an indication that they passed, says a resolution the AMA Medical Student Section presented at the Special Meeting. Residency programs and applicants could benefit from clarity in how those indicators will be reviewed and assessed, the resolution says.
To that end, delegates directed the AMA to work with appropriate stakeholders to release guidance for residency and fellowship program directors on equitably comparing students who received three-digit USMLE Step 1 or COMLEX Level 1 scores and students who received pass-fail scores.
Level the playing field for DOs on away rotations
Students from osteopathic medical schools are at a competitive disadvantage in securing elective experiences—such as away rotations typically offered during the fourth year of undergraduate medical education—at some allopathic medical schools. So concludes an AMA Council on Medical Education report adopted at the AMA Special Meeting.
That reality could translate to less exploration of specialties and less opportunity as residency applicants. To remedy this inequity, the House of Delegates adopted new policy to encourage:
- The Association of American Medical Colleges to request that its member institutions promote equitable access to clinical electives for allopathic and osteopathic medical students and charge equitable fees to visiting allopathic and osteopathic medical students.
- The Accreditation Council for Graduate Medical Education to require its accredited programs to work with their respective affiliated institutions to ensure equitable access to clinical electives for allopathic and osteopathic medical students and charge equitable fees to visiting allopathic and osteopathic medical students.
Delegates also modified existing policy to encourage “equitable access to, and equitable fees for, clinical electives for allopathic and osteopathic medical students.”
Transparency a must on loan forgiveness for medical student debt
The nation’s physician workforce needs and the weight of medical student-loan debt cannot be ignored, says an AMA Council on Medical Education report presented at the AMA Special Meeting. According to the Association of American Medical Colleges, the typical medical student-loan debt in 2019 was $200,000. Meanwhile, people from historically marginalized racial and ethnic groups carry higher levels of medical student-loan debt compared with the overall population.
To address this growing burden on future physicians, delegates adopted new policy to:
- Encourage key stakeholders to collect and disseminate data on the impacts of medical education debt on career choice, especially with regard to the potentially intersecting impacts of race or ethnicity, socioeconomic status, and other key sociodemographic factors.
- Monitor new policies and novel approaches to influence career choice based on the key factors that affect the decision to enter a given specialty and subspecialty.
The HOD also amended existing policy regarding the Public Service Loan Forgiveness (PSLF) program, calling on the AMA to:
- Monitor the denial rates for physician applicants to the PSLF.
- Undertake expanded federal advocacy—in the event denial rates for physician applicants are unexpectedly high—to encourage release of information on the basis for the high denial rates, increased transparency and streamlining of program requirements, consistent and accurate communication between loan servicers and borrowers, and clear expectations regarding oversight and accountability of the loan servicers responsible for the program.
- Work with the U.S. Department of Education to ensure that applicants to the PSLF and its supplemental extensions, such as Temporary Expanded Public Service Loan Forgiveness (TEPSLF), are provided with the necessary information to successfully complete either program in a timely manner.
- Work with the Department of Education to ensure that people who would otherwise qualify for PSLF and its supplemental extensions, such as TEPSLF, are not disqualified from the program.
AMA: Health financing bias exacerbates rural health inequities
Rural Americans suffer significant and unacceptable health inequities compared with their urban counterparts, evidenced by mortality rates that are 23% higher and preventable hospitalizations that are 40% higher across all racial and age groups, according to a resolution presented by the Iowa delegation AMA Special Meeting. Moreover, rural health inequities have been worsening for the last 30 years.
One significant contribution to this inequity is the chronic shortage of physician specialists and limited doctor availability in rural areas, which is exacerbated by biases in Medicare payment models that dissuade physicians from practicing in rural areas and discourage those in urban areas from seeing rural patients through telehealth.
The House of Delegates directed the AMA to “recognize that systemic bias in health care financing has been one of many factors leading to rural health disparities and advocate for elimination of these biases through payment policy reform to help reduce the shortage of rural physicians and eliminate health inequities in rural America.”
“Vast rural areas disproportionately struggle to care for the sickest of patients, experience a dearth of primary health care professionals, and endure strenuous, disruptive financial burdens,” said AMA President Gerald E. Harmon, MD. “Until the systemic bias in health care funding is recognized, a viable model for reducing or eliminating rural health disparities cannot move forward.”
Account for people with Middle Eastern and North African descent
When it comes to the U.S. Census, the National Institutes of Health, and other surveys that collect demographic data in the U.S., people of Middle Eastern and North African descent are not recognized as belonging to a unique, independent racial category.
The absence of this racial designation category has had a profound limiting effect on research and has perpetuated a cycle of undocumented health inequities for this population, says an AMA Resident and Fellow Section resolution presented at the Special Meeting.
The House of Delegates took action on the issue, and the AMA will:
- Add “Middle Eastern/North African (MENA)” as a separate racial category on all AMA demographics forms.
- Advocate the use of “Middle Eastern/North African (MENA)” as a separate race category in all uses of demographic data, including but not limited to medical records, government data collection and research, and within medical education.
- Study methods to further improve disaggregation of data by race which most accurately represent the diversity of our patients.
“Physicians benefit from collecting accurate patient demographic data and applying it to medical research, personalized health care, and patient-centered engagement,” said AMA Trustee Willarda V. Edwards, MD, MBA.
“Expanding the demographic classification to recognize people of Middle Eastern and North African descent can help inform efforts to eliminate health care inequities, an important priority for the AMA and our nation,” Dr. Edwards added. “By revising standards to reflect our changing demographics and how our patients self-identify, we can better examine quality data stratified by race and ethnicity with improved accuracy.”
Trainees who call out unsafe conditions shouldn’t see retaliation
When physicians across the country brought attention to unsafe working conditions or inadequate personal protective equipment (PPE), many were disciplined, harassed, ignored or fired.
Similarly, many medical trainees do not have process protections, which means they may be disciplined or terminated for issues unrelated to academic or clinical performance, says a resolution presented by the AMA Resident and Fellow Section during the Special Meeting.
The House of Delegates directed the AMA to:
- Review reports of unsafe working conditions and unfair retaliation for public expression of safety concerns on the part of physicians and trainees and consider methods to provide logistical and legal support to such aggrieved parties
- Develop and distribute guidance on how physicians and trainees may make public comments on working conditions and legal options to promote workplace safety (for example, filing formal OSHA complaints), as well as other workplace protection issues as appropriate.
In addition, delegates amended existing policy to ensure it addresses trainees. As amended, the policy calls on the AMA to:
- Advocate that it is the responsibility of health care facilities to provide sufficient personal protective equipment for all employees and staff, as well as trainees and contractors working in such facilities, in the event of a pandemic, natural disaster, or other surge in patient volume or PPE need.
- Support the rights of physicians and trainees to participate in public commentary addressing the adequacy of clinical resources or health and environmental safety conditions necessary to provide appropriate and safe care of patients and physicians during a pandemic or natural disaster.
Lastly, the HOD adopted new policy to support:
- The inclusion of health care workers in workplace protections and programs generally applicable to employees in other sectors, barring extenuating circumstances and evidence-based reasoning supporting otherwise.
- Legislation and other policies protecting physicians and trainees from violence and unsafe working conditions.
Monday, Nov. 15
AMA sets out to strengthen U.S. public health systems
Prior to the COVID-19 pandemic, organizations that represent U.S. governmental public health agencies had cautioned that their ability to keep the country safe from disease and public health emergencies was constrained by lack of dedicated and sustained funding.
The nation’s public health infrastructure has also been threatened by high rates of staff turnover as well as obsolete data-collection and reporting methods. These obstacles can lead to delayed detection and response to public health threats, says an AMA Council on Science and Public Health report adopted at the Special Meeting.
“The COVID-19 pandemic did not create these problems, but it inarguably exposed the cracks that had long existed in our public health infrastructure,” says the report. “For decades, public health professionals have been advocating for greater resources to plan and prepare for just such a crisis.”
Read more about the House of Delegates' actions to strengthen public health systems.
Give doctors, med students with disabilities a stronger advocacy base
Some 85 million people in the U.S. have a disability, yet many medical facilities lack the resources to adequately treat them. This is simply for want of accommodations, such as a ramp or adequately sized hallways, says an AMA Board of Trustees report that delegates adopted at the Special Meeting.
There are professional organizations such as the Association of Medical Professionals with Hearing Loss and the Society of Healthcare Professionals with Disabilities, but “their reach tends to be limited and information and resources for physicians may be hard to come by, particularly in times of crisis or emergency,” the Board of Trustees report says.
To reduce stigma and promote the inclusion of physicians and medical students with disabilities, the House of Delegates directed the AMA to:
- Establish an advisory group composed of AMA members who themselves have a disability to ensure additional opportunities for including physicians and medical students with disabilities in all AMA activities.
- Promote and foster educational and training opportunities for AMA members and the medical community at large to better understand the role disabilities can play in the health care work environment, including cultivating a rich understanding of so-called invisible disabilities for which accommodations may not be immediately apparent.
- Develop and promote tools for physicians with disabilities to advocate for themselves in their own workplaces, including a deeper understanding of the legal options available to physicians and medical students to manage their own disability-related needs in the workplace.
- Communicate to employers and medical staff leaders the importance of including within personnel policies and medical staff bylaws protections and reasonable accommodations for physicians and medical students with visible and invisible disabilities.
Push for resident and fellow physicians’ access to retirement plans
Resident and fellow physicians are often overwhelmed with student-loan debt following the completion of medical school, so it is imperative that they prepare for their futures as early as they can by paying down debt, saving for retirement and making other sound financial decisions. Yet employment benefits packages at graduate medical education institutions are notoriously uneven.
“While some teaching institutions offer benefit packages including retirement plans with matching contributions, many do not, and funds are limited,” says an AMA Board of Trustees report adopted at the Special Meeting. “Similarly, while some institutions provide financial education and advising, many do not, and many trainees are left feeling ill-prepared and unsettled when it comes to their financial security.”
To help set future physicians on the right financial path, the House of Delegates adopted policy to “support the availability of retirement plans for residents and fellows at all teaching institutions that are no less favorable than those offered to other institution employees.”
Delegates also amended existing policy to encourage “teaching institutions to offer retirement plan options, retirement plan matching, financial advising and personal finance education.”
Over 29 million still uninsured. Here’s how to help cover them.
Passage of the American Rescue Plan Act, COVID-19 relief legislation enacted earlier this year, has shifted the dynamics of U.S. health care coverage by increasing the generosity of and expanding eligibility for financial help to buy health insurance via Affordable Care Act (ACA) marketplaces. But additional steps can be taken to make affordable health insurance available to many more of the estimated 28.9 million who remain uninsured, says an AMA Council on Medical Service report adopted at the Special Meeting.
“We find ourselves in a time that we can cover the remaining uninsured in this country,” AMA Trustee David H. Aizuss, MD, said in a statement. “By closing the coverage gap, fixing the family glitch, and helping workers and their families who are facing unaffordable employer coverage, most of the nation’s uninsured will be eligible for ACA financial assistance, either the form of premium tax credits or Medicaid/CHIP. We can capitalize on this financial help available to cover the remaining uninsured.”
Read more about the AMA's road map to help cover the remaining uninsured.
Address Medicare patients’ end-of-life care needs
Except under very limited circumstances, Medicare patients in need of custodial care at the end of their lives are prohibited by Medicare from electing skilled nursing facility (SNF) and hospice benefits at the same time for the same condition. Physicians are regularly challenged to find placements for terminally ill patients who need more care than can be provided at home but cannot afford the costs of nursing care or stays at a care facility.
“Research has suggested that—of the large numbers of patients enrolled in the SNF benefit at the end of their lives—many would have elected hospice if they had not needed room and board coverage,” says an AMA Council on Medical Service report presented at the Special Meeting.
The council's report recognizes the need for supportive care services among many end-of-life patients and the importance of discharging these patients to appropriate settings with necessary, affordable supports. The costs and benefits of care models incorporating elements of SNF and hospice care are worthy of further study.
To that end, AMA delegates adopted new policy to support:
- Medicare coverage of—and appropriate payment for—supportive care services, including assistance with activities of daily living, as needed, under Medicare’s hospice benefit.
- That the Centers for Medicare & Medicaid Services’ study and pilot-test care models that allow concurrent use of Medicare’s hospice and SNF benefits for the same condition.
- Increased access to comprehensive, interdisciplinary palliative care services by Medicare patients in skilled nursing facilities.
Improve care for patients dually eligible for Medicare, Medicaid
Integrating care for patients who are eligible for both Medicare and Medicaid has been difficult due in part to their complex and diverse needs and the involvement of siloed government health programs that were not designed to work together.
Essential criteria for developing successful integrated care programs are outlined in an AMA Council on Medical Service report whose recommendations were adopted at the Special Meeting.
In comparison to Medicare enrollees, a greater share of dual-eligible patients come from historically marginalized racial and ethnic groups, are women, or have disabilities. So reducing inequities in health and access to care must be considered by integrated-care models if they are to improve quality of life quality and health outcomes over the long term.
To address these challenges, the AMA House of Delegates adopted new policy to support integrated care for people who are dually eligible for Medicare and Medicaid.
Such integrated care should align with AMA policy and meet the following criteria:
- Care is grounded in the diversity of dually eligible enrollees and services are tailored to individuals’ needs and preferences.
- Coverage of medical, behavioral health and long-term services and supports is aligned.
- Medicare and Medicaid eligibility and enrollment processes are simplified, with enrollment assistance made available as needed.
- Enrollee choice of plan and physician is honored, allowing existing patient-physician relationships to be maintained.
- Services are easy to navigate and access, including in rural areas.
- Care coordination is prioritized, with quality case management available as appropriate.
- Barriers to access, including inadequate networks of physicians and other providers and prior authorizations, are minimized.
- Administrative burdens on patients, physicians and other providers are minimized.
- Educational materials are easy to read and emphasize that the ability and power to opt in or out of integrated care resides solely with the patient.
- Physician participation in Medicare or Medicaid is not mandated, nor are eligible physicians denied participation.
Over 96% of doctors are vaccinated. Follow their lead.
More than 96% of practicing physicians have been fully vaccinated against COVID-19, according to an AMA national survey (PDF) conducted in June. The survey found no significant regional differences in vaccination rates. Of physicians not yet fully vaccinated, 45% said they did plan to get vaccinated.
“Practicing physicians across the country are leading by example, with an amazing uptake of the COVID-19 vaccines,” said Susan R. Bailey, MD, when the survey’s findings were released. Dr. Bailey is the AMA’s immediate past president.
The AMA has developed a COVID-19 vaccines guide for physicians to promote factual vaccine information online that includes sample social media posts and messages.
Learn more about what doctors wish patients knew about COVID-19 vaccine boosters, and check out all the entries in the AMA’s What Doctors Wish Patients Knew™ series.
Also read this Leadership Viewpoints column by AMA President Gerald E. Harmon, MD, on how to seize the opportunity to vaccinate younger kids against COVID-19.
Sunday, Nov. 14
Reference committees continue work today
The following reference committees will meet from 9 a.m.–12:30 p.m. CST:
- Reference Committee E, which covers science and technology.
- Reference Committee G, which covers medical practice.
Watch this short video, from 2019, to learn more about how AMA policy is made.
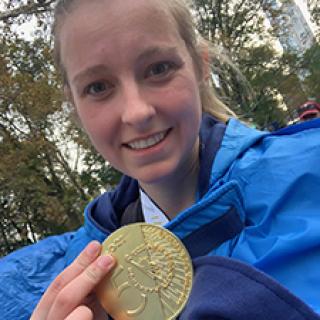
She ran an AMA section meeting, then a marathon
Any organized medicine policymaking meeting can seem, at times, as exhausting as running a marathon. For AMA Medical Student Section (AMA-MSS) Vice-Speaker Whitney Stuard, it was just the prelude to the real thing.
Stuard, a medical student at the University of Texas Southwestern Medical Center, co-presided over the section meeting last weekend with AMA-MSS Speaker Sally Midani. Then came race day—Sunday, Nov. 7—when Midani presided so Stuard could take part in the New York City Marathon. Thanks to careful planning, the two were able to carry off a seamless section meeting along with the other medical students.
Preparing for the AMA-MSS meeting was actually “more exhausting” than training for the marathon, Stuard said of her third time running in a 26.2-mile foot race.
“I really wanted Sally’s and my first meeting to go smoothly,” Stuard said. “We had a large amount of business to complete and many hardworking authors and MSS members there to discuss resolutions. Our MSS did a fantastic job getting through discussions and having a meaningful debate.”
“Once business was through, I felt excited and motivated to go run the marathon,” she added. “It was as if completing one challenge made me even more energized to complete the second challenge.”
Stuard finished the New York City race with a personal-best time of 4 hours and 54 minutes.
Read more about the November 2021 AMA-MSS Meeting.
Watch these education sessions on demand
Several of the meeting’s education sessions were recorded ahead of time and you can watch them at your convenience. Among them:
- “Issues of ethical importance: Health care for pediatric LGBTQ+ patients.”
- “Compassionate care starts with us: Educating medical students on working with patients with intellectual or developmental disabilities.”
- “Medical misinformation gone viral: The science of misinformation spread and how to combat it.”
- “Educating low-literacy patients to understand health insurance systems post-passage of the Affordable Care Act.”
- “A pandemic within a pandemic: Using telehealth to recognize the signs of intimate partner violence.”
- “Developing communication standards between providers and Arab Immigrants/Refugees.”
Saturday, Nov. 13
Reference committees start today
AMA delegates will offer testimony today and tomorrow on the dozens of reports and resolutions up for consideration at the meeting. Delegates draw on their expertise, the best evidence in the medical and health policy literature, and the insights of their state medical associations and national medical specialty societies to weigh in on proposals that address issues affecting patients and physicians.
These reference committees will meet 9 a.m.–12:30 p.m. CST today:
- Reference Committee A, which covers medical service.
- Reference Committee D, which covers public health.
- Reference Committee F, which covers AMA governance and finance.
From 1–5 p.m., these reference committees also will meet:
- Reference Committee on Amendments to Constitution & Bylaws, which covers the AMA constitution, bylaws and medical ethics matters.
- Reference Committee B, which covers legislation.
- Reference Committee C, which covers medical education.
Discover AMA advocacy on COVID-19 and more
Throughout the COVID-19 pandemic, the AMA has been the leading physician and patient ally—voicing recommendations to key congressional leaders and agency staff, state policymakers and private sector stakeholders.
Check out this updated dashboard to find out more about the AMA’s recent and ongoing COVID-19 advocacy efforts.
Also see this resource that tracks AMA’s 2020–2021 advocacy efforts across a range of issues, including Medicare physician payment, scope of practice, surprise billing, medical liability reform and more.
And make sure to check out the “AMA COVID-19 Update,” a series of YouTube episodes that shows how the AMA is supporting America’s physicians and medical students as safe and effective vaccines in the U.S. prevent illnesses and deaths.
Also worth watching is the new “AMA Moving Medicine” video series, which amplifies physician voices and highlights developments and achievements throughout medicine. The series provides practical advice and expert insights on today’s leading health care issues.
Both programs also are available in audio-only format through your favorite podcast-listening service, along with many other original podcasts from the AMA.
Updates from AMA groups and sections
AMA member groups and sections representing medical students, residents and fellows, and many others across career stages, special interests and more held the November 2021 AMA Section Meetings last week.
These meetings of the AMA sections offer physicians and medical students the opportunity to influence policy, attend educational programs and network.
Discover what each group or section has learned and accomplished at their virtual meetings:
- AMA Academic Physicians Section
- AMA Advisory Committee on LGBTQ Issues
- AMA Integrated Physician Practice Section
- AMA International Medical Graduates Section
- AMA Medical Student Section
- AMA Minority Affairs Section
- AMA Organized Medical Staff Section
- AMA Private Practice Physicians Section
- AMA Resident and Fellow Section
- AMA Senior Physicians Section
- AMA Women Physicians Section
- AMA Young Physicians Section
Friday, Nov. 12
Patients still trust doctors. Learn why doctors count on the AMA.
While the public’s trust in many institutions has waned during the COVID-19 pandemic, people still trust their doctors—and doctors trust the AMA. Executive Vice President and CEO James L. Madara, MD, provided proof of this trust in an address during the opening session of the AMA Special Meeting, and he explained that the AMA had earned that trust by being physicians’ powerful ally in patient care. (Read the speech.)
“Trust in physicians was shown to be high among all groups, demographics and political affiliations,” Dr. Madara told delegates. “Physicians trust us to give voice to their concerns, and to help mitigate the challenges they face—from PPE shortages, to financial stress, to increasing regulatory burdens.”
Read more from Dr. Madara about how the AMA benefits the public by being the physicians’ powerful ally in patient care.
AMA president: Physicians are leading “an army against the virus”
A former career officer in the U.S. Air Force and the Air National Guard, Gerald E. Harmon, MD, recognized the strained looks he saw in the hospital, working with young physicians and residents as COVID-19 ravaged his community hospital in Georgetown County, South Carolina, this past summer.
“The fear and weariness in young clinicians’ faces was not unlike what I witnessed in the medical arena in Iraqi Freedom and Enduring Freedom after 9/11—I’d call it battle fatigue,” Dr. Harmon said at tonight's opening session. “Like combat, the unrelenting demands of responding to COVID patients has led to physical and emotional exhaustion and pushed physicians and our entire health care workforce to the breaking point.” (Read the speech.)
Learn more from Dr. Harmon about how the AMA helps give doctors the tools they need to fight COVID-19 and tackle other longstanding challenges.
Making doctors’ voices the loudest in the room
During the November 2021 AMA Section Meetings’ plenary session, seven outstanding AMA members focused on the need to elevate physician voices to protect patients and the nation's health.
The pandemic has revealed so much about the expertise and resilience of our nation’s physicians—but it has also revealed the need, now more than ever, for elevating their voices. When it comes to medicine, the AMA believes physician voices should be the loudest in the room—and the AMA is working hard to make that happen.
After remarks from AMA President Gerald E. Harmon, MD, and AMA Board of Trustees Chair Bobby Mukkamala, MD, special guest Peter Hotez, MD, PhD, discussed his experiences dispelling anti-vaccine myths as a vaccinologist and the father of a child with autism.
“There was a void and there was a place for a physician-scientist to say: Hey, wait a minute. This is not reality—here’s the reality,” said Dr. Hotez, dean of the National School of Tropical Medicine, and professor of pediatrics and molecular virology and microbiology at Baylor College of Medicine.
Then, a panel of four members of the AMA Ambassador Program offered their advice to doctors nationwide on how to elevate physician voices individually and as a profession.
Read more about the plenary session, which covered six ways doctors can use their voices to help science get heard, or watch below.
Quick links for the meeting
These essentials will help you get the most out of the November 2021 AMA Special Meeting.
- Access the reports and resolutions delegates will consider, as well as reference committee reports and final actions as they become available.
- Get instructions to navigate the virtual House of Delegates and reference committee hearings.
- Search the AMA Pictorial Directory to find your peers and stay connected before, during and after the AMA Special Meeting (AMA members only).
- Find out how to claim AMA PRA Category 1 Credit™ for the eligible education sessions held during the meeting.
Follow the meeting on social media
Highlights of the meeting’s key moments and House of Delegates policy actions will be posted daily at the AMA website, the November 2021 AMA Special Meeting website, and the AMA’s Facebook page, Instagram and Twitter account using #AMAmtg.
Addresses from leadership and more will be featured on the AMA’s YouTube channel. After the meeting, be sure to follow the AMA on LinkedIn for additional updates as well.
Top 10 issues at the AMA Special Meeting
Nearly 700 physicians, residents and medical students are gathering—virtually—over five days for the November 2021 AMA Special Meeting to consider proposals across a wide range of clinical practice, payment, medical education and public health topics.
Among the notable issues:
- Strengthening U.S. public health infrastructure and opposing limits placed on public health authorities.
- Combating public health disinformation.
- Enhancing privacy for people who use mail-order DNA testing kits.
- Limiting the authority to grant medical exemptions for vaccinations.
- Improving maternal health and eliminating maternal health inequities.
- Refining recommendations for evidence-based policing reform.
- Ensuring that a diverse range of skin tones is represented in dermatology medical education.
- Requiring health insurer transparency regarding patients’ out-of-pocket costs for individual prescription drugs.
- Bolstering the physician workforce in rural communities.
- Advocating for heat exposure protections for outdoor workers.