Can physicians be held liable in cases in which they’ve never treated the patients experiencing the adverse outcome?
That’s a question that is increasingly being put before the courts, and one explored during a recent education session held by the Litigation Center of the American Medical Association and State Medical Societies.
The mission of the Litigation Center is to represent the interests of the medical profession in the courts. It brings lawsuits, files amicus briefs and otherwise provides support or becomes actively involved in litigation of general importance to physicians.
The Litigation Center held a moot court session in which it presented arguments from Warren v. Dinter, a case in which a physician was held liable for harm to patient he had never examined, reviewed her records or spoke to her directly.
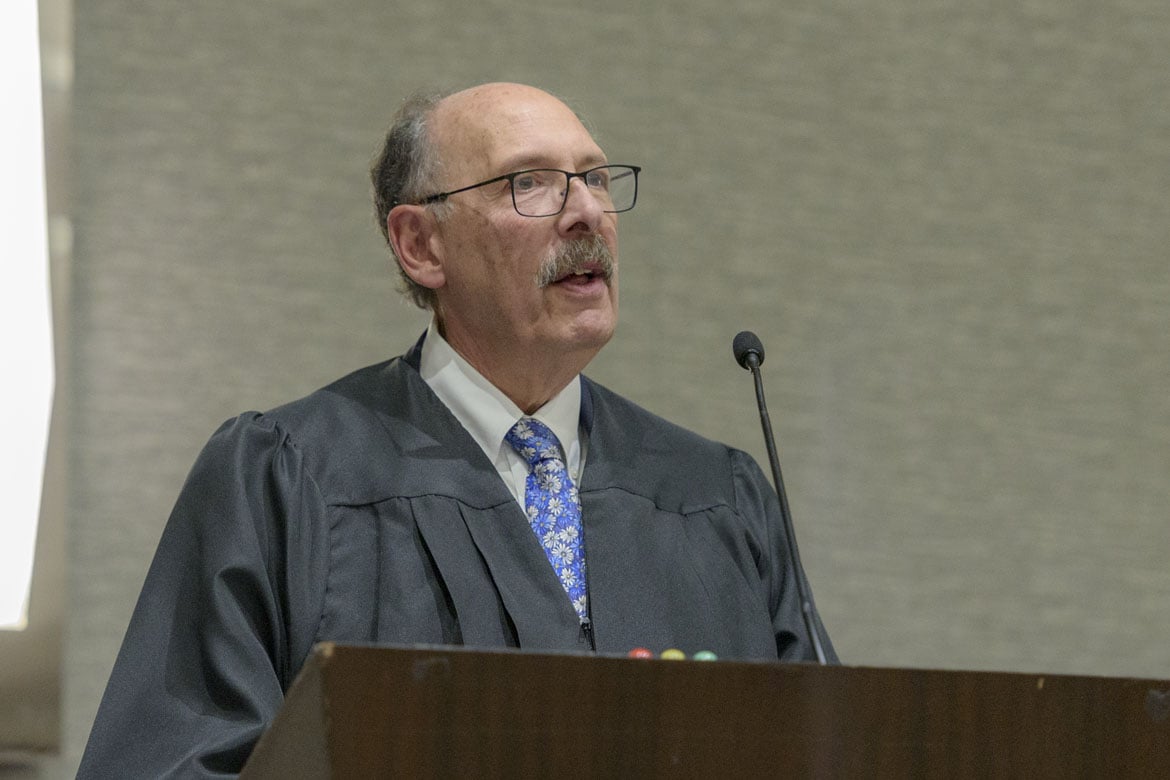
Arguments were presented by Leonard Nelson, director of the Litigation Center, and Mark R. Whitmore, a Minnesota attorney who wrote the amicus brief in the case. Jack R. Bierig, the AMA’s principal outside counsel for more than 40 years, played the role of the Minnesota Supreme Court with the help of the audience.
At issue was whether Dr. Dinter had “legal duty of care” even though he never examined the patient, viewed her record or spoke to her directly. He received a phone call from a nurse practitioner (NP) who consulted him on whether a patient should be admitted.
Nurse practitioners can practice independently in Minnesota, but the NP in this case did not have hospital admitting privileges. After their conversation, Dr. Dinter surmised that the patient’s symptoms were due to diabetes which could be managed at home. She later died from sepsis.
While the NP could not have had the patient admitted, Whitmore noted that she could have directed the patient to the hospital emergency department.
The Litigation Center, in the amicus brief written by Whitmore and filed with the Minnesota Medical Association and the Minnesota Hospital Association, argued that the duty of care was premised on a patient-physician relationship.
The state district and appellate courts held the same position, with the court of appeals noting that it was desirable policy to promote informal consultations among health care professionals. They feared that, if such consultations could lead to malpractice liability, doctors might refuse to take such calls.
The Minnesota Supreme Court, however, highlighted Dr. Dinter’s role as the hospital “gatekeeper,” and said this role outweighed the traditional patient-physician relationship. It also ruled that, in Minnesota, duty of care was based on “foreseeability of harm” and it reversed the appellate court ruling in an April 17 decision.
During the session, which took place during the 2019 AMA Interim Meeting, audience members expressed their concerns and views on the chilling effect of the decision, decision-making authority of NPs and physician assistants, legal ethics and medical ethics, telemedicine and the overall importance of good communication.
AMA Attorney Erin Sutton noted that the Litigation Center has received an “overwhelming response” regarding the case and that similar cases involving physician liability regarding patients they have not seen are popping up across the country.