In order to help physicians and other providers, the Centers for Medicare & Medicaid Services (CMS) has expanded its Accelerated and Advance Payment Program for the duration of the public health emergency. CMS is authorized to provide accelerated or advance payments during the period of the public health emergency to any Medicare physician, provider or supplier who submits a request to the appropriate Medicare Administrative Contractor (MAC) and meets the required qualifications. This is also included in the Coronavirus Aid, Relief and Economic Security (CARES) Act.
To qualify for advance/accelerated payments physicians, providers or suppliers must:
- Have billed Medicare for claims within 180 days immediately prior to the date of signature on the physician’s request form
- Not be in bankruptcy
- Not be under active medical review or program integrity investigation
- Not have any outstanding delinquent Medicare overpayments
Amount of payment for physicians: Qualified physicians will be asked to request a specific amount using an Accelerated or Advance Payment Request form provided on each MAC’s website. Most physicians will be able to request up to 100% of the Medicare payment amount for a previous three-month period. The amount requested must be a good faith estimate; it does not have to be perfect.
Processing time: Each MAC will work to review and issue payments within seven calendar days of receiving the request. (Some MACs have made it possible to submit the requests on weekends.)
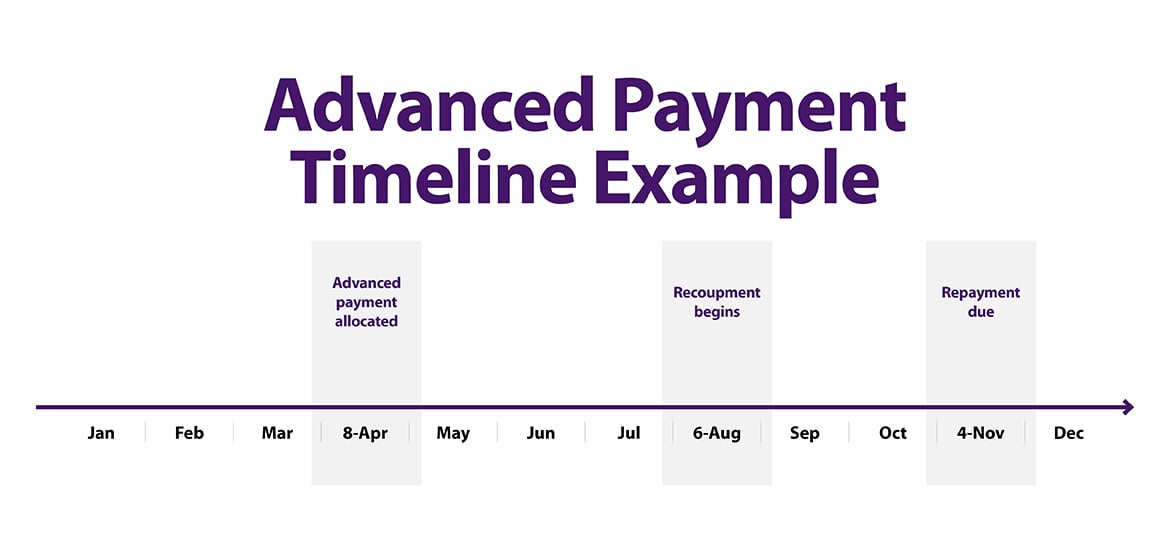
Repayment: CMS has extended the repayment of these accelerated/advance payments to begin 120 days after the date of issuance of the payment. Physicians billing under Part B will have 210 days from the date of the accelerated or advance payment was made to repay the balance.*
Recoupment and reconciliation: Physicians can continue to submit claims as usual after the issuance of the accelerated or advance payment; however, recoupment will not begin for 120 days. Physicians will receive full payments for their claims during the 120-day delay period. At the end of the 120-day period, the recoupment process will begin and every claim submitted by the physician will be offset from the new claims to repay the accelerated/advanced payment. Thus, instead of receiving payment for newly submitted claims, the physician’s outstanding accelerated/advance payment balance is reduced by the claim payment amount. This process will be automatic.
The request form and more information on the process will also be available on each MAC’s website. When determining a payment amount to request, physicians should consider that their Medicare fee-for-service payments will be automatically reduced starting four months after the payment is issued for up to three months or until repayment is met. Below is a hypothetical timeline depicting an advanced payment issued in the beginning of April, recoupment beginning in August, and repayment due in early November.
How to request accelerated or advance payment
- Complete and submit a request form: Accelerated/Advance Payment Request forms vary by contractor and can be found on each individual MAC’s website. Complete the form and submit it to your MAC via mail or email. CMS has established COVID-19 hotlines at each MAC that are operational Monday – Friday to assist you with accelerated payment requests. You can contact the MAC that services your geographic area.
- Refer to the CMS Medicare contracting guide (PDF) to locate your designated MAC.
- What to include in the request form: Incomplete forms cannot be reviewed or processed, so it is vital that all required information is included with the initial submission. The physician must complete the entire form, including the following:
- Legal business name/ Legal name
- Correspondence address
- National Provider Identifier (NPI)
- Other information as required by the MAC
- Amount requested based on your need: Most physicians will be able to request up to 100% of the Medicare payment amount for a three-month period.
- Reason for request: Physicians should check box 2 (“Delay in provider/supplier billing process of an isolated temporary nature beyond the provider’s/supplier’s normal billing cycle and not attributable to other third-party payers or private patients.”). Also, state that the request is for an accelerated/advance payment due to the COVID19 pandemic.
- Who must sign the request form: The form must be signed by an authorized representative of the provider/supplier.
- How to submit the request form: While electronic submission will significantly reduce the processing time, requests can be submitted to the appropriate MAC by fax, email or mail. You can also contact the MAC helplines listed above.
- Do provider/suppliers have any appeal rights: Providers/suppliers do not have administrative appeal rights related to these payments. However, administrative appeal rights would apply to the extent CMS issued overpayment determinations to recover any unpaid balances on accelerated or advance payments.
Additional documents
List of Medicare administrative contractors
- CGS Administrators, LLC (CGS) - Jurisdiction 15 (KY, OH, and home health and hospice claims for the following states: DE, DC, CO, IA, KS, MD, MO, MT, NE, ND, PA, SD, UT, VA, WV, and WY) Toll-free hotline telephone number: 1-855-769-9920. Hours of operation: 7 a.m. – 4 p.m, CT. Toll-free hotline number for home health and hospice claims: 1-877-299- 4500. Hours of operation: 8:00 am – 4:30 p.m. CT for main customer service; 7 a.m. – 4 p.m. CT for Electronic Data Interchange (EDI).
- First Coast Service Options Inc. (FCSO) – Jurisdiction N (FL, PR, US VI) Toll-free hotline telephone number: 1-855-247-8428 hours of operation: 8:30 a.m. – 4:00 p.m. ET.
- National Government Services (NGS) – Jurisdiction 6 & Jurisdiction K (CT, IL, ME, MA, MN, NY, NH, RI, VT, WI, and home health and hospice claims for the following states: AK, AS, AZ, CA, CT, GU, HI, ID, MA, ME, MI, MN, NH, NV, NJ, NY, MP, OR, PR, RI, US VI, VT, WI, and WA). Toll-free hotline telephone number: 1-888-802-3898. Hours of operation: 8 a.m. – 4 p.m.CT.
- Novitas Solutions, Inc. –Jurisdiction H & Jurisdiction L (AR, CO, DE, DC, LA, MS, MD, NJ, NM, OK, PA, TX, (includes Part B for counties of Arlington and Fairfax in VA and the city of Alexandria in VA). Toll-free hotline telephone number: 1-855-247-8428. Hours of operation: 8:30 a.m. – 4:00 p.m. ET.
- Noridian Healthcare Solutions - Jurisdiction E & Jurisdiction F (AK, AZ, CA, HI, ID, MT, ND, NV, OR, SD, UT, WA, WY, AS, GU, MP). Toll-free hotline phone number: 1-866-575-4067. Hours of operation: 8 a.m. – 6 p.m. CT.
- Palmetto GBA - Jurisdiction J & Jurisdiction M (AL, GA, NC, SC, TN, VA (excludes Part B for the counties of Arlington and Fairfax in VA and the city of Alexandria in VA), WV, and home health and hospice claims for AL, AR, FL, GA, IL, IN, KY, LA, MS, NM, NC, OH, OK, SC, TN, and TX). Toll-free hotline phone number: 1-833-820-6138. Hours of operation: 8:30 a.m. – 5 p.m. ET.
- Wisconsin Physician Services (WPS) - Jurisdiction 5 & Jurisdiction 8 (IN, MI, IA, KS, MO, NE) toll-free hotline. Telephone number: 1-844-209-2567. Hours of operation: 7 a.m. – 4 p.m. CT.
- Noridian Healthcare Solutions, LLC – DME A & D (CT, DE, DC, ME, MD, MA, NH, NJ, NY, PA, RI, VT, AK, AZ, CA, HI, ID, IA, KS, MO, MT, NE, NV, ND, OR, SD, UT, WA, WY, AS, GU, MP). Toll-free hotlines: A: 1-866-419-9458; D: 1-877-320-0390. Hours of operation: 8 a.m. – 6 p.m. CT.
- CGS Administrators, LLC – DME B & C (AL, AR, CO, FL, GA, IL, IN, KY, LA, MI, MN, MS, NM, NC, OH, OK, SC, TN, TX, VA, WI, WV, PR, US VI). Toll-free hotline telephone numbers: B: 866-590-6727; C: 866-270-4909. Hours of operation: 7 a.m. – 4 p.m. CT.
- What the CARES Act means for physicians & medical students
- CARES Act: AMA COVID-19 pandemic telehealth fact sheet
- CARES Act: Loans & other financial assistance for physician practices
- CARES Act: Medicare’s COVID-19 advance payment program FAQ
*The AMA is seeking additional clarity on repayments, as it seems possible that a physician who receives 3 months advance payments and then has them recouped over 3 months (beginning 120 days later) may not receive any Medicare revenue during that subsequent 3-month period. It is not clear that this is CMS’ intention.